Archive for the ‘Mass Litigation’ Category
What we learned at the DRI Nursing Home/ALF Litigation Seminar
Monday, October 16th, 2017
What we learned at the DRI Nursing Home/ALF Litigation Seminar
Every year, we look forward to the DRI Nursing Home/ALF Litigation Seminar to collaborate with leaders on the newest trends and strategies in the long-term care industry. Each session gives our team an opportunity to access cutting-edge information related to the latest changes in legislation and clinical management strategies.
Here are a few of our favorite sessions from the DRI Nursing Home/ALF Litigation in Atlanta, Georgia this year:
Managing Wound Care Risk Exposure with Karen Lou Kennedy-Evans
Karen Lou Kennedy-Evans’ session offered an interesting perspective on the evolution of a clinical concept involving the use of the laboratory values albumin and prealbumin. As legal nurse consultants responsible for investigating pressure injury claims, often times we see albumin and prealbumin levels used by counsel to make a point about the stability or instability of a resident’s nutritional status. Karen’s talk however emphasized the importance of examining the serum albumin levels in consideration of the overall morbidity and mortality of the resident, versus any possible nutrition issue.
It is really helpful for our team of nurses to hear perspectives such as this from leaders in the industry, like Karen, who are able to identify what’s important clinically and what’s not in building a defense. As fellow clinicians involved in long-term care case reviews, we appreciate her perspective in helping us stay focused on the important issues at hand and how we can best use that information to strengthen our defense.
Defending the Elopement and Fall Case: Tips and Tools that Must be Part of your Defense with Frank Alvarez and Ashlee Gray
For long term care facilities, it’s extremely important to have an elopement strategy and to perform elopement drills for preventative management. During this session, Frank Alvarez and Ashlee Gray emphasized how many nursing homes don’t have a comprehensive elopement plan in place and of those that do, many do not routinely drill the plan with the staff. They reiterated the importance of why it’s essential to properly assess a resident’s elopement risk and implement risk reduction strategies. At ALN Consulting, we echo this sentiment. We have seen many instances of elopement result in tragedy for residents of skilled nursing homes with subsequent filing of legal claims with potentially substantial settlements. We cannot stress enough how important it is for facilities to develop elopement strategies, document those strategies and practice elopement drills consistently.
Stage IV – F314 and the Four-Prong Test for Defending Pressure Ulcers with Aimee Garcia
During this session, Aimee Garcia did an excellent job outlining alternative theories for unavoidable skin breakdown. Dr. Garcia emphasized that it’s extremely important for the defense team to understand clinical unavoidability and how to use this concept to help craft a defense strategy. She reiterated how important it is for the defense team to investigate how well facilities evaluate the resident’s risk for skin breakdown. Other key takeaways include: implementing appropriate interventions for prevention and management of skin breakdown, monitoring the impact of those interventions, and revising the plan where appropriate. Overall, prevention is the goal in minimizing skin breakdown.
ALN Consulting continues to become a growing force in the industry. We are proud to be a part of the DRI community, and appreciate opportunities like the Nursing Home/ALF Litigation Seminar to strengthen our partnerships in the industry and network with our long term care colleagues. The ALN Consulting team is a leading provider of medical-legal consulting services nationwide. Contact us today to add our expertise to your next case.
What the Mirena IUD Case Means for Expert Testimony
Monday, June 5th, 2017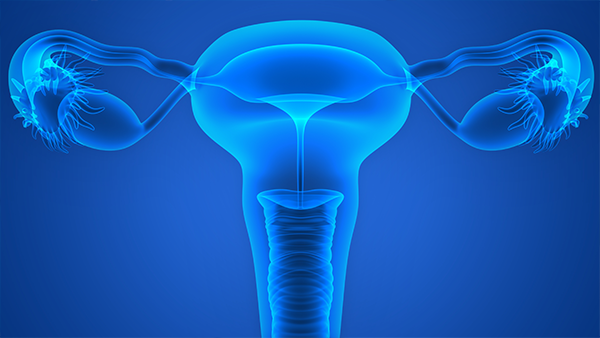
In 2011, the first personal injury complaint was made against Mirena, a plastic intrauterine device (IUD) used by over 2 million women worldwide. Manufactured by Bayer Healthcare Pharmaceuticals, one of the world’s largest pharmaceutical companies, Mirena is a T-shaped IUD coated with the hormone levonorgestrel. Designed to offer up to five years’ protection against unintended pregnancies, it is Bayer’s most popular IUD model and marketed as safe and effective.
Yet over a thousand women came forward alleging that Mirena can migrate once it is inserted into the uterus – perforating the uterus or cervix. Lawsuits allege that Bayer failed to adequately warn doctors and women about the risk of uterine perforation. Most of these women sued Bayer rather than their personal medical professionals. Their attorneys took the position that their medical side effects come from the IUD itself and not from an OB-GYN error in inserting the device.
The plaintiffs also claimed that Mirena’s label was misleading: it did not specify any necessary action other than having a doctor confirm the device’s placement. It only identified uterus perforation as a risk during the insertion, but not afterward. They allege that Bayer failed to warn patients of the risks associated with the IUD.
While marketing the drug, Bayer Healthcare sponsored “Mirena Parties” at which a nurse would make a scripted presentation on the benefits of using this IUD. Some plaintiffs claim that the different risks associated with its use were never elaborated upon. After these “parties” made their rounds, the FDA warned Bayer in writing that their marketing campaign was misrepresenting the issues with Mirena and to modify their advertising and presentations. This 2009 correspondence stated that the company had overstated Mirena’s efficiency, omitted information about its risk, and ultimately made a serious of false or misleading statements in its advertising.
Three years later, a study found that nearly half of doctors were not informed of the risks associated with the device. Bayer’s legal position, on the other hand, was that it was not aware of those side effects at the time of the marketing campaign and that they did not act irresponsibly.
Quality in expert witnesses
Expert witnesses were poised to testify that Mirena could cause uterine perforation after being inserted. The judge, however, found that these witnesses’ opinions were not supported by scientific literature and had been developed for the purpose of the lawsuit. In doing so, the defendants’ motion successfully barred these expert witnesses from even testifying.
Without established experts supporting their case, plaintiff attorneys countered that experts weren’t really needed to establish general causation. But the problem was that they had already named some to support their case. The court decided that it was well beyond the common understanding of lay jurors to discuss the uterus’s anatomy, the strength of its muscles, and the medical ramifications that could be caused by an IUD insertion procedure, and how existing technology could spot them. Thus, an expert on general causation testimony was not simply optional. So when plaintiff counsel claimed that the Mirena IUD lawsuits were “simple soft-tissue cases” that didn’t require expert opinions, their argument fell flat.
The plaintiffs also tried to argue that a series of purported party admissions of wrongdoing under 801(d)(2) could substitute for the required expert proof. The court, however, found that to substitute for expert testimony, it would have to be “the clearest and most unambiguous admission that the product or device in question can cause the alleged injury.” After walking through each case claiming a defendant admission, the plaintiff attorneys’ arguments still fell far short. Both individually and collectively, these admissions weren’t sufficiently clear, concrete, or detailed “to permit a jury to consider intelligently the existence, or not, of secondary perforation.”
The Mirena plaintiffs argued that the jury could and should assess what the defendants’ statements actually meant. But again, without expert testimony, a jury coming out of the general population could not be expected to have either the scientific or medical background to accurately evaluate these statements. They would speculate about whether a medical procedure could have caused the patients’ injuries, even though they had no information or training with which to make an informed decision.
This type of speculation is precisely why expert testimony is required. Without it, no jury would have a sound basis to find in favor of plaintiffs. The plaintiffs’ counsel had nothing to show they could carry their burden on general causation. A judgment was entered in favor of the defendant in all of the cases – all 1300 of them.
Legal nurse consultants: bridging the gap
How could things go so wrong for the plaintiffs when they had a damning FDA letter and study that supported their case? Clearly, drug and medical device causation calls for quality expert testimony that cannot be easily challenged in a court of law. And when it comes to medical negligence, so many health issues – both physical and emotional – are challenging to quantify.
Here is where a legal nurse consultant’s expertise is of particular value. Upon studying the files and medical records, this uniquely qualified consultant can formulate his or her own conclusions and recommend the right specialists for the case – from medical specialists to ancillary professionals like physical therapists and pharmacists. For a case like IUD negligence, an LNC would find an expert witness in obstetrics and gynecology. This OB-GYN would need to be familiar with the specific brand in order to explain that device’s specifics and any follow-up treatment. The LNC may also research literature and product issues relevant to the impending lawsuit.
With accusations of improper warnings, a legal nurse consultant can recruit a medical device labeling expert to explain the proper procedures and any existing warnings for the device. A mental health expert can best help lay jurors appreciate the full impact of the defendants’ error on the plaintiff’s life and well-being. Most importantly, both the LNC and the expert witnesses would convey both the causation and its consequences in terms that any member of the jury could understand.
While it is true that these professionals are hired to work for healthcare organizations as risk managers or risk reduction experts, they are also an enormous boon for mass torts and class action lawsuits, as well as individual suits. Legal nurse consultants are in a unique position to build the strongest, most manageable court case for their clients – and seek justice and relief for individuals who have suffered due to medical negligence.
Sources
- https://www.masstortnexus.com/mass-torts-news/federal-court-reopens-mirena-iud-product-liability-mdl/
- http://www.thenationaltriallawyers.org/2013/04/mass-tort-likely-over-mirena-iud-injuries/
- https://www.druganddevicelawblog.com/2016/08/summary-judgment-for-all-pending-cases-in-the-mirena-mdl.html
- https://www.theexpertinstitute.com/mirena-iud-a-mass-tort-primer/
- http://www.foxnews.com/health/2016/07/29/judge-rules-against-some-1300-lawsuits-over-bayers-mirena-iud.html
- http://www.youhavealawyer.com/mirena/
- https://www.law360.com/articles/792741/bayer-wants-all-mirena-iud-cases-tossed-for-lack-of-experts
- https://lawstreetmedia.com/issues/health-science/legal-battles-mirena-iud-whats-next/
Baby Powder Mass Tort Litigation: Strong Scientific Foundation or Just a Cloud of Dust?
Wednesday, April 26th, 2017
To first understand this subject, one needs to understand mass tort. You may have heard of a class-action lawsuit and associate the terminology with a mass tort lawsuit, but these are two separate types of cases despite implied similarities. Both types of cases involve a large number of individuals who claim to have been harmed by a common entity. The difference lies in procedurally how the plaintiffs are represented (Ashcraft and Gerel, LLP, n.d.). For class-action lawsuits, a firm files the lawsuit on behalf of all of those harmed, as one plaintiff with one trial; while for mass tort lawsuits, plaintiffs are treated individually, with separate trials (Rottenstein Law Group, LLP, n.d.). To proceed as a class action lawsuit, the Court must approve the claim as dictated by Rule 23 of the Federal Rules of Civil Procedure which states that:
- the class is so numerous that joinder of all members is impracticable;
- there are questions of law or fact common to the class;
- the claims or defenses of the representative parties are typical of the claims or defenses of the class; and
- the representative parties will fairly and adequately protect the interests of the class (Ashcraft and Gerel, LLP, n.d.).
If the Court does not approve the claim to proceed as a class action lawsuit, then the plaintiffs can individually proceed with mass tort litigation, each having their own trial in their own jurisdiction (Rottenstein Law Group, LLP, n.d.). In either case, firms may utilize mass media for advertisement to make the general public aware of possible harmful effects of a product or device. The firms may also use advertising to alert potential plaintiffs that claims are being filed, to gain more clients, and to make potential jurors aware, all in an indirect effort to gain victory.
In 2009, one of the first cases was filed, alleging that women’s genital use of talcum powder or baby powder has led to diagnoses of ovarian cancer, which in some cases, has proceeded to wrongful death.
One may ask, “how on earth can something applied to the outside of the body cause cancer in tissues located on the inside of the body?” The answers have taken years to prove, yet Cramer, Vitonis, Terry, Welch, and Titus (2016) explain that research on this very topic began back in the 1960’s, when there was the discovery that talcum powder contained asbestos—a current, well-known carcinogen (Cralley, Key, Groth, Lainhart, & Ligo, 1968; Graham & Graham, 1967). The group also explain the progression of scientific research demonstrating the link and cause of talcum/baby powder to ovarian cancers listing dozens of more studies. The literature review identifies specific risk factors and associations.
Essentially, the established facts are:
- Talc has fine particles which migrate through the vaginal canal, the cervical opening, the uterus and fallopian tubes to the ovaries, causing cellular changes predisposing a woman to cancer.
- The longer a woman has utilized genital-area application of talc (talc years), the more at-risk she is for cancer. There does not appear to be a correlation with the cornstarch variation of baby powder.
- There is an association between talc users and asthma; therefore, those who ended up with ovarian cancer also report having had a history of asthma.
- Other contributing factors point to an influence involving estrogen and/or prolactin in talc-users: pre-menopausal women, post-menopausal women who used hormone therapy, obese pre-menopausal women, and those who breastfed, currently smoke, or use alcohol.
- There seems to be a higher association among African American or Black women.
- The pathologic tissue subtypes of epithelial ovarian cancer which were more likely talc-associated, “include serous and mucinous borderline tumors and invasive serous and endometrioid tumors” (Cramer, Vitonis, Terry, Welch, & Titus, 2016, p. 345).
With mass tort litigation involving large numbers of plaintiffs, with vast medical histories and substantial medical records, it is crucial to utilize a staff which can efficiently organize, review, and analyzes the enormous associated files. It takes a group of professionals who are educated to assess and evaluate the case files for completeness, and who can perform critical thinking and analysis. The medical-legal professionals at ALN Consulting, perform this type of work, and more, every day. At ALN Consulting, we do more than help you prepare…we prepare you to win.
References
Ashcraft and Gerel, LLP. (n.d.). Class action vs. mass tort: a brief explanation [web page]. Retrieved from http://ashcraftandgerel.com/attorney-blogs/class-action-vs-mass-tort-a-brief-explanation/
Cralley, L. J., Key, M. M., Groth, D. H., Lainhart, W. S., & Ligo, R. M. (1968). Fibrous and mineral content of cosmetic talcum products. American Industrial Hygiene Association Journal, 29(4), 350-354.
Cramer, D. W., Vitonis, A. F., Terry, K. L., Welch, W. R. & Titus, L. J. (2016). The association between talc use and ovarian cancer: A retrospective case–control study in two US states. Epidemiology, 7(23), 334-346.
Graham, J., & Graham, R. (1967). Ovarian cancer and asbestos. Environmental Research, 1(2), 115-28.
Rottenstein Law Group, LLP. (n.d.) What is a “mass tort” [web page]. Retrieved from http://www.rotlaw.com/legal-library/mass-torts/
ALN Litigation Perspective
Monday, October 3rd, 2016
Fudge & McArthur, P.A.’s Donna Fudge and Benjamin Broadwater announce victory in recent Stage IV Pressure Ulcer/Nursing Home case in Florida.
The complexity of circumstances demonstrated in this case is not atypical of the facts in many of the long-term care cases in litigation today. The importance of cohesion between the medical and legal defense teams cannot be emphasized enough in these cases. From both a clinical and legal standpoint, considerable skills are required to weed through the minutia of what was likely an abundance of medical records and break down the case facts simply into a bad outcome despite the rendering of good care. Of significance in this case was the team’s ability to use the medical record to create the picture of collaborative care provided in the absence of wound documentation. Unfortunately, all too often we see key portions of the medical record are missing, requiring our nurse consultants to hunt for the pieces of the puzzle necessary to reconstruct the plan of care and develop a fail-safe defense strategy.
Defense Jury Verdict: Morgan & Morgan, P.A. represented the Estate of Willie F. Coley, in a lawsuit against TR & SNF, Inc., d/b/a The Nursing Center at University Village, and BVM Management, Inc. in relation to Mr. Coley’s 12+ year residency at University Village’s skilled nursing facility. The Complaint alleged negligence for the development of a Stage IV sacral/coccyx pressure ulcer. Mr. Coley passed away 15 months after leaving University Village and continued to have this pressure ulcer until the time of his death. A graphic photograph of the Stage IV ulcer was shown to the Jury.
This case focused on the final three months of Mr. Coley’s 12+ year residency at University Village. Plaintiff alleged that University Village failed to implement appropriate interventions after re-admission from a hospital stay, and failed to revise any interventions after Mr. Coley developed his sacral/coccyx ulcer, in violation of the Federal Regulation for pressure ulcers, FTag 314. Plaintiff also alleged that the caregivers failed to follow the Facility’s own Policies and Procedures by failing to monitor/track the wound, and by failing to provide adequate pressure relief every 2 hours. As a result, Plaintiff alleged that University Village failed to prevent the development, and worsening, of Mr. Coley’s pressure ulcer. Lastly, Plaintiff alleged that the University Village caregivers failed to properly assess and treat Mr. Coley for Pain allegedly associated with his wound
Defense Themes: The defense focused on Mr. Coley’s 10 most recent Hospitalizations leading up to his coccyx skin wound and his 20 underlying Comorbidities including a history of cerebrovascular accident, stercoral ulcer, dementia, paralysis, C. difficile, and GERD which contributed to Mr. Coley’s development and eventual worsening of his sacral/coccyx ulcer. The Defense proved that proper interventions were put in place when Mr. Coley was re-admitted from the hospital, but despite these interventions, Mr. Coley experienced an unavoidable “Friction Blister” that progressed to a pressure ulcer and eventually became a Stage IV with suspected osteomyelitis. The jury heard expert testimony that the healing of Mr. Coley’s left and right Buttocks skin wounds, adjacent to his Coccyx sore, was evidence that he was being properly offloaded in that area. The Defense argued that it met FTag 314 by: (1) evaluating Mr. Coley’s risk factors for additional pressure sores, (2) implementing interventions for the prevention of pressure sores, (3) monitoring the impact of those interventions by notifying the physicians of changes in the wound and obtaining new treatment orders such as a wound vac and an infectious disease consult, and (4) revising those interventions.
Overcoming Documentation Problems: The nursing home had lost its wound tracking documentation. However, the Defense argued that any lack of documentation did not mean that there was a lack of monitoring. The staff consistently notified Mr. Coley’s physicians of changes in the wound’s condition, and a wound care physician was tracking the wound on a weekly basis from April 23, 2014 through June 4, 2014. The Defense pointed out to the jury that Plaintiff’s allegations were based on records that were “cherry picked” and it was explained that, in order to get a true and accurate understanding of the interventions such as re-positioning, pain management and wound monitoring by the caregivers, the jury had to look at the entirety of Mr. Coley’s Chart, which was filled with evidence that these areas of care were actually provided.
Jury Verdict: Following the 5 day jury trial, the jury returned a defense jury verdict in favor of both Defendants.
Trial Team: Donna Fudge and W. Benjamin Broadwater of Fudge & McArthur, P.A. were lead trial counsel. Caitlin Kramer, Esq., and Paralegals Amy Bozarth and Julie Christ of Fudge & McArthur, P.A. assisted in the trial.
Defense Experts: Dr. Aimee Garcia (Houston, Texas) and Alexa Parker Clark (St. Petersburg, Florida)
It’s the complex cases such as this one which demonstrate the essential need for synergy between the medical and legal defense teams. ALN Consulting’s team of experts are trained to quickly identify key pieces of evidence that are missing or have been falsified. We can piece together a solid picture from numerous records, giving legal teams a clear path to case resolution.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.
Identifying Medical Malpractice Expert Witnesses
Monday, June 6th, 2016
Sometimes medical negligence is apparent without need for explanation. It doesn’t take an expert to find fault when someone operates on the wrong limb or administers the wrong medication to a nursing home resident.
If medical professionals are the only ones with control over a negative outcome, and when an adverse event could only have been caused by a medical error, our legal system invokes the doctrine of res ipsa loquitur (Latin for “the thing speaks for itself.”) Simply stated, res ipsa is the principle noting that an event could have happened only due to negligence.
Although personal injury laws and rules of evidence are determined at the state level, the elements of res ipsa are pretty standard. For a case to meet the doctrine of res ipsa loquitur, three factors must be present: 1) the event would not occur in the absence of negligence; 2) the evidence of negligence rules out the possibility that the plaintiff’s actions caused the adverse event; and, 3) the negligent act occurs within the context of care provided by the defendant. It is often recommended that an expert witness be consulted, even in a case of res ipsa. The defendant’s attorney will usually challenge the notion that he or she had complete control over the circumstances.
In most cases of medical or nursing home negligence, expert witnesses are necessary to move a case forward. Lack of expert testimony can mean an early decision in an opponent’s favor – if not an outright dismissal. The facts and language of medicine are often too complex to understand. The appointed expert will walk the jury through the maze of medicine to understand why a lawsuit was filed in the first place.
Most states require plaintiffs to consult an expert witness to determine if the medical care provided to the plaintiff met the standard of care. In the legal arena, the standard of care is the level at which the average, prudent provider in a given community would practice. It is how similarly qualified practitioners would have managed the patient’s care under the same or similar circumstances. The standard of care is not necessarily the best care – just the average level expected of any care provider.
When a case does require qualified professional expertise, both plaintiffs and defendants must hire someone to serve in the role of expert witness. For cases to be tried in Federal Court, the Federal Rules of Civil Procedure (Fed.R. Civ.P.), requires the selected expert to prepare a detailed report in addition to a list of the expert’s prior testimony and compensation.
Although some states follow the Federal Rules of Civil Procedure, others have different rules for dealing with experts. In some states, an expert witness will be deposed before trial so the opposing side can be fully prepared to counter his or her opinions. In others, like New York, a legal team is not required to disclose the name of the designated expert, but they do have to provide opposing counsel with the expert’s bibliography.
What Makes A Medical Professional An Expert?
You may ask, “What makes a medical professional an expert?” One legal dictionary defines an expert as “a person who through education or experience has developed skill or knowledge in a particular subject so that he or she may form an opinion that will assist the fact finder.”
Each state has its own definition of who may be designated as a medical expert. Some states require that professional experience must be current, either for a specified number of years or that the expert was practicing in a clinical setting at the time of the incident. A degree from an AMA or AOA-accredited medical school are common requirements, as is board certification in the experts’ area of expertise. An unrestricted medical license with no recent history of suspension or revocation is paramount. Many states mandate that potential experts must devote a certain percentage of professional time to an active clinical practice, to avoid earning the reputation as a “professional witness.”
Nurse expert witnesses typically need a B.S.N. and recent clinical expertise in the same area as the defendant, with no record of legal issues or board disciplinary actions. Certification in the expert’s nursing specialty is an added plus.
Some states adhere to different versions of a specialty rule, which requires experts to practice in the same field of medicine as the defendant physician or nurse. A state’s locality rule obligates claimants to prove, by expert testimony, the recognized standard of acceptable professional practice in the community where the defendant medical provider practices or a similar community. For example, many states require that potential expert witnesses in medical malpractice cases must come from the state in which the alleged incident occurred or from a state contiguous to the venue in which the alleged incident occurred.
In most state malpractice lawsuits, attorneys on both sides will know the witnesses’ identities before getting to trial. They will research each expert’s career from their education to their publications. Every statement in an article written or testimony in cases with similar issues will be carefully scrutinized. The legal team will research the facts on which each claim is based – gleaning all it can to uncover the weak link in an expert’s opinion.
How Can An Expert Witness Be Utilized?
Expert witnesses can be used in a variety of ways. A medical professional may appear before the court as a “fact witness.” A “fact witness” is called to explain the medicine to the judge and jury. His or her role is to provide “just the facts” about a case, with no opinion regarding the medical care provided.
In medical malpractice and nursing home litigation, causation is the common Achilles’ heel. The rub lies in two questions every medical malpractice suit must answer. First, did the defendant fail to follow the standard of care for professionals in his or her position?
To answer this, a plaintiff-appointed expert may cite medical board guidelines or publications. What would industry standards expect of the defendant? How would a conscientious colleague with the same training treat this patient? What issues would that medical professional check for, and how would those issues be treated if diagnosed? An expert witness need not practice a higher standard of care than the defendant. He or she must only be conversant enough to determine that this standard was not followed.
The second question is thornier. If there was a breach in the standard of care, did this breach cause the negative outcome or damages? Given all the factors present, how likely was the plaintiff’s injury a result of substandard care?
The plaintiff’s goal is to find an expert who believes there is evidence of a breach of the standard of care. The defense will use its own expert to establish that the standard of care was observed – or that any deviation did not directly or proximately cause the adverse event. The plaintiff’s attorney, in turn, will get to work uncovering every possible way to challenge the defense’s expert testimony.
Finding properly credentialed healthcare professionals who are willing to offer opinions is not always easy. So what’s the best way to choose an expert witness? By consulting one.
Here is where a nurse’s expertise is of particular value. Upon studying the files and medical reports, this uniquely qualified consultant can recommend appropriate specialists.
Nursing expertise is ideal in complex cases of medical and care negligence. Identifying the probable cause of a medical event takes more than simply checking blood pressure and vital signs. A nurse is interested not only in physical agility but whether the patient has followed doctors’ and therapists’ directives and asked for assistance when necessary. This expert not only researches a patient’s diet, but whether or not the patient has adhered to the diet or eaten the food provided in a hospital or care facility. He or she would review physician progress notes, consultation reports, nursing progress notes, patient teaching records, lab results for specific issues and medication history for germane clues.
Legal nurse consultants (LNCs) are generally brought in to determine the merit of a case. Some help attorneys formulate questions to be asked at a deposition or trial. Some LNCs provide both consultation and testimony, while others prefer to work “behind the scenes.”
LNCs play a vital and advantageous role finding other experts for the case – from M.D. specialists to ancillary professionals like physical therapists, respiratory therapists, and pharmacists. Nurse expert witnesses are expected to testify at a deposition and trial if needed. Unlike the LNC consulting expert, the testifying expert may or may not be required to put their opinion in writing.
Both consulting LNCs and nurse expert witnesses review medical records and deposition testimony and formulate their conclusions. They commonly organize pertinent medical records and prepare record chronologies or timelines. They may also research medical and nursing literature and standards germane to issues in the suit brought forth. Both kinds of experts offer their own unique value to legal teams – and are often hired by healthcare organizations as risk managers or compliance experts.
As with other litigation, medical malpractice and long-term care cases often pit one expert against the other. Sometimes the tipping point in a jury’s decision is how well one witness can translate technical intricacies in to language they understand. ALN Consulting’s team of nurse consultants are in a unique position to build the strongest, most manageable court case for their clients – and boil medical-legal issues down to their essence. Contact us to learn how!
The Power of a Nurse’s Words
Wednesday, March 23rd, 2016
We here at ALN sometimes encounter a sense of “Am I making a difference and is it enough?” in our profession. And it’s interesting to hear that same thing from other nurses. Diane M Goodman recently posted a piece that so compelled us, we just had to share. Thank you, Diane.”
Sticks and Stones; The Power of a Nurse’s Words
By Diane M. Goodman, Originally appeared in MedScape, Jan 21, 2016
Many of us were raised in a generation by mothers who warned us of the old English adage about taunting others through the use of name-calling and words. We knew better. Words could either be unbelievably comforting or leave lasting scars on our memories.
As nurses, our words and our voices are no less profound. We can change the trajectory of a life by coaxing change from a desultory or despondent patient, and we can inspire peers to greatness when they feel they cannot work another moment or another busy day.
Sharing research with peers may allow them to comprehend the improbability of what we DO on a daily basis. By reading a quantitative time-study, for example, and sharing it with colleagues, they may have an improved understanding of why nurses need stress management techniques to perform their jobs. Nursing is extremely difficult work. Expecting substantive conversation or specific phrases to “just happen” at the bedside is like asking the typical pilot to land an airplane on the Hudson!
Nurses, on the average, complete >70 (!!) tasks per hour. Nurses change tasks approximately every 55 seconds. They are also interrupted approximately once every 32 minutes, with the highest amount of interruptions recorded during medication administration!*
Why is it important to know this? While this time/event study was conducted in Sydney, the research was rigorous enough to be utilized internationally as an example of why nurses may find it “difficult” to bond with patients. We may be groping to find the right words to instill initiative, hope, and change in our patients. We could even be struggling a bit.
Nina (not her real name) reminded me of this in ICU. I was struggling. She was paralyzed, intubated, ventilated, and so, so sick. I was sure she would not survive. She was only 19.
I was exhausted every night, hanging more blood, platelets and medications than I had ever hung in my life. She was septic and she had leukemia. “Sticks and stones”, I repeated in my head over and over, warning myself not to frown or sigh, or show tiredness EVER. Instead, I stroked her hair, and told her how much I loved my little sister, and my dogs. I played music for her when my voice got tired or I ran out of words. If nothing sweet or positive was left to be said, I smiled and hummed, night after exhausting night. OK, so I did a lot of humming.
Her bed was empty one night, as ICU beds often are. Rehab, they said. Long-term. Newer, sicker patients came and went.
Six months later, a young, attractive woman was wheeled in with a huge family circling her, including one very determined sister. It was Nina. She remembered nothing of her stay but a woman who stroked her hair and hummed and talked softly of dogs and family. I would have given her almost zero odds of surviving, and here she was!! Sitting tall, with very little residual effects. I couldn’t believe she remembered me! She remembered nothing else.