Archive for the ‘Pharma’ Category
Medicinal Marijuana Linking to Decline in Overdoses
Friday, August 19th, 2016
The Washington Post reports that University of Georgia researchers have produced significant evidence linking prescription marijuana to falling overdose statistics in states where medicinal marijuana use is legal.
The study suggests that chronic pain sufferers can find alternatives to dangerous medication on a large scale. While this development hasn’t come without push back from pharmaceutical lobbyists, states that have legalized medical marijuana have already seen a plunge in painkiller prescriptions.
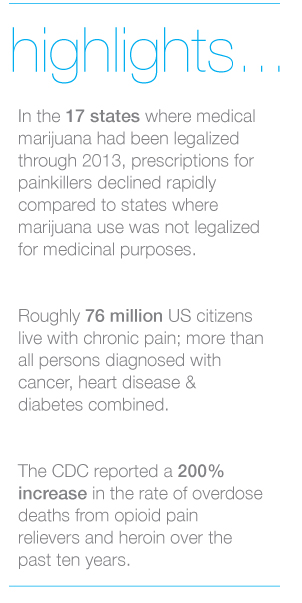
The Georgia researchers reported that in the 17 states where medical marijuana use had been legalized through 2013, prescriptions for painkillers and other classes of medications declined rapidly compared to states where marijuana use was not legalized for medicinal purposes. The number of prescriptions for medications commonly used to treat chronic pain, such as antidepressants, anti-nausea, anti-anxiety and seizure medications decreased across the board. However, the most striking finding was the consistent drop in prescriptions written for analgesics or painkillers.
 The study conducted by the University of Georgia researchers adds more information to the rapidly growing pool of knowledge supporting marijuana use for treatment of chronic pain, both in combination with opioids and as a viable treatment on its own.
The study conducted by the University of Georgia researchers adds more information to the rapidly growing pool of knowledge supporting marijuana use for treatment of chronic pain, both in combination with opioids and as a viable treatment on its own.
Chronic pain is common, multidimensional and individualized and treatment can be challenging for healthcare providers as well as patients. Roughly 76 million US citizens live with chronic pain; a number larger than all persons diagnosed with cancer, heart disease and diabetes combined.
In March of this year, the Centers for Disease Control and Prevention (CDC) updated guidelines for clinicians who prescribe opioids for individuals suffering from chronic pain.
The guidelines help providers make informed decisions about pain treatment for patients 18 and older in primary care settings. The CDC recommendations focus on the use of opioids in treating chronic pain and are not intended for patients actively being treated for cancer and those receiving palliative or end-of-life care.
Unlike cannabis, opioids carry a known risk of chemical dependence. Over ten years ago, the CDC reported a 200% increase in the rate of overdose deaths from opioid pain relievers and heroin.
This finding has several implications for the investigation of medical malpractice cases. Where cannabis is not legally available, patients may increasingly seek it on the black market and complicate a medical investigation. The full ramifications of medically prescribed cannabis may not be known for many years, and with decreasing revenue at stake, the pharmaceutical industry continues to fund studies discounting its benefits. Most immediately, the role of prescription drugs in a case is affected by the state in which an adverse medical event took place. Finding expert witnesses conversant in drug laws of that state will be more important than ever.
ALN Consulting can research, identify and secure expert witnesses appropriate for cases involving the use of medical marijuana and other pain treatments. We do more than help you prepare…we prepare you to win, call us today.
Opioid Use and Abuse
Monday, June 27th, 2016
With the death of Prince from an overdose of the narcotic Fentanyl, another celebrity becomes a statistic in the opioid drug overdose epidemic, currently gripping the United States. This epidemic is responsible for nearly half a million deaths between 2000 to 2014, according to the Centers for Disease Control and Prevention (CDC). Increases in prescription opioid analgesics and heroin deaths are thought to be the forces fueling the epidemic.
Opioid Use – A Dangerous Trend
Since 2000, the CDC reports a 200% increase in the rate of overdose deaths related to the use of opioid pain relievers and heroin, the main drugs associated with overdose deaths. During that time period, death rates from opioid overdoses increased significantly for both sexes, in persons aged 25–44 years and those older than 55 years of age. The states of West Virginia, Ohio, Kentucky, New Mexico and New Hampshire are the most affected.
Natural and semisynthetic opioids, which include the most commonly prescribed opioid pain relievers, oxycodone and hydrocodone, continue to be involved in more overdose deaths than any other opioid type. One component of opioid overdoses is believed to involve illicitly-made fentanyl, a short-acting opioid.
Heroin-related deaths increased in recent years. A history of misuse of prescription opioids is the strongest risk factor for heroin initiation and use. Increased availability of heroin, its relatively low price compared to prescription opioids and high purity appear to be major drivers of the upward trend in heroin use, overdoses, and deaths.
New Guidelines
On March 15, 2016, just weeks before Prince’s death, the CDC released its Guideline for Prescribing Opioids for Chronic Pain – United States 2016. The guideline was developed to assist primary care providers in ensuring the safest and most effective treatment for their patients with chronic pain which is not related to active cancer treatment, palliative and end-of-life care.
The guideline presents twelve recommendations for providers who manage chronic pain patients. Arguably, the most important guideline recommendation is the endorsement of nonopioid therapy as the preferred method of dealing with chronic pain. The use of opioids should be limited to situations when the benefits for alleviating pain and improving function outweigh the risks of opioid use. And when opioid analgesics are prescribed, it is recommended that providers prescribe the lowest dose found to be an effective treatment of an individual’s pain. Frequent follow-up and evaluation of the drug treatment plan is suggested. The guideline encourages the provider to become a partner with the patient in developing treatment goals and outline how the opioids will be discontinued if no benefit is achieved. The CDC Guideline can be accessed at http://www.cdc.gov/drugoverdose/prescribing/guideline.html.
If you or someone you know suffers from an opioid addiction, please consider contacting SAMHSA’s National Helpline for help or reach out to the National Institute on Drug Abuse.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. ALN Consulting can assist your defense team with finding the documentation to strengthen your case.
Identifying Medical Malpractice Expert Witnesses
Monday, June 6th, 2016
Sometimes medical negligence is apparent without need for explanation. It doesn’t take an expert to find fault when someone operates on the wrong limb or administers the wrong medication to a nursing home resident.
If medical professionals are the only ones with control over a negative outcome, and when an adverse event could only have been caused by a medical error, our legal system invokes the doctrine of res ipsa loquitur (Latin for “the thing speaks for itself.”) Simply stated, res ipsa is the principle noting that an event could have happened only due to negligence.
Although personal injury laws and rules of evidence are determined at the state level, the elements of res ipsa are pretty standard. For a case to meet the doctrine of res ipsa loquitur, three factors must be present: 1) the event would not occur in the absence of negligence; 2) the evidence of negligence rules out the possibility that the plaintiff’s actions caused the adverse event; and, 3) the negligent act occurs within the context of care provided by the defendant. It is often recommended that an expert witness be consulted, even in a case of res ipsa. The defendant’s attorney will usually challenge the notion that he or she had complete control over the circumstances.
In most cases of medical or nursing home negligence, expert witnesses are necessary to move a case forward. Lack of expert testimony can mean an early decision in an opponent’s favor – if not an outright dismissal. The facts and language of medicine are often too complex to understand. The appointed expert will walk the jury through the maze of medicine to understand why a lawsuit was filed in the first place.
Most states require plaintiffs to consult an expert witness to determine if the medical care provided to the plaintiff met the standard of care. In the legal arena, the standard of care is the level at which the average, prudent provider in a given community would practice. It is how similarly qualified practitioners would have managed the patient’s care under the same or similar circumstances. The standard of care is not necessarily the best care – just the average level expected of any care provider.
When a case does require qualified professional expertise, both plaintiffs and defendants must hire someone to serve in the role of expert witness. For cases to be tried in Federal Court, the Federal Rules of Civil Procedure (Fed.R. Civ.P.), requires the selected expert to prepare a detailed report in addition to a list of the expert’s prior testimony and compensation.
Although some states follow the Federal Rules of Civil Procedure, others have different rules for dealing with experts. In some states, an expert witness will be deposed before trial so the opposing side can be fully prepared to counter his or her opinions. In others, like New York, a legal team is not required to disclose the name of the designated expert, but they do have to provide opposing counsel with the expert’s bibliography.
What Makes A Medical Professional An Expert?
You may ask, “What makes a medical professional an expert?” One legal dictionary defines an expert as “a person who through education or experience has developed skill or knowledge in a particular subject so that he or she may form an opinion that will assist the fact finder.”
Each state has its own definition of who may be designated as a medical expert. Some states require that professional experience must be current, either for a specified number of years or that the expert was practicing in a clinical setting at the time of the incident. A degree from an AMA or AOA-accredited medical school are common requirements, as is board certification in the experts’ area of expertise. An unrestricted medical license with no recent history of suspension or revocation is paramount. Many states mandate that potential experts must devote a certain percentage of professional time to an active clinical practice, to avoid earning the reputation as a “professional witness.”
Nurse expert witnesses typically need a B.S.N. and recent clinical expertise in the same area as the defendant, with no record of legal issues or board disciplinary actions. Certification in the expert’s nursing specialty is an added plus.
Some states adhere to different versions of a specialty rule, which requires experts to practice in the same field of medicine as the defendant physician or nurse. A state’s locality rule obligates claimants to prove, by expert testimony, the recognized standard of acceptable professional practice in the community where the defendant medical provider practices or a similar community. For example, many states require that potential expert witnesses in medical malpractice cases must come from the state in which the alleged incident occurred or from a state contiguous to the venue in which the alleged incident occurred.
In most state malpractice lawsuits, attorneys on both sides will know the witnesses’ identities before getting to trial. They will research each expert’s career from their education to their publications. Every statement in an article written or testimony in cases with similar issues will be carefully scrutinized. The legal team will research the facts on which each claim is based – gleaning all it can to uncover the weak link in an expert’s opinion.
How Can An Expert Witness Be Utilized?
Expert witnesses can be used in a variety of ways. A medical professional may appear before the court as a “fact witness.” A “fact witness” is called to explain the medicine to the judge and jury. His or her role is to provide “just the facts” about a case, with no opinion regarding the medical care provided.
In medical malpractice and nursing home litigation, causation is the common Achilles’ heel. The rub lies in two questions every medical malpractice suit must answer. First, did the defendant fail to follow the standard of care for professionals in his or her position?
To answer this, a plaintiff-appointed expert may cite medical board guidelines or publications. What would industry standards expect of the defendant? How would a conscientious colleague with the same training treat this patient? What issues would that medical professional check for, and how would those issues be treated if diagnosed? An expert witness need not practice a higher standard of care than the defendant. He or she must only be conversant enough to determine that this standard was not followed.
The second question is thornier. If there was a breach in the standard of care, did this breach cause the negative outcome or damages? Given all the factors present, how likely was the plaintiff’s injury a result of substandard care?
The plaintiff’s goal is to find an expert who believes there is evidence of a breach of the standard of care. The defense will use its own expert to establish that the standard of care was observed – or that any deviation did not directly or proximately cause the adverse event. The plaintiff’s attorney, in turn, will get to work uncovering every possible way to challenge the defense’s expert testimony.
Finding properly credentialed healthcare professionals who are willing to offer opinions is not always easy. So what’s the best way to choose an expert witness? By consulting one.
Here is where a nurse’s expertise is of particular value. Upon studying the files and medical reports, this uniquely qualified consultant can recommend appropriate specialists.
Nursing expertise is ideal in complex cases of medical and care negligence. Identifying the probable cause of a medical event takes more than simply checking blood pressure and vital signs. A nurse is interested not only in physical agility but whether the patient has followed doctors’ and therapists’ directives and asked for assistance when necessary. This expert not only researches a patient’s diet, but whether or not the patient has adhered to the diet or eaten the food provided in a hospital or care facility. He or she would review physician progress notes, consultation reports, nursing progress notes, patient teaching records, lab results for specific issues and medication history for germane clues.
Legal nurse consultants (LNCs) are generally brought in to determine the merit of a case. Some help attorneys formulate questions to be asked at a deposition or trial. Some LNCs provide both consultation and testimony, while others prefer to work “behind the scenes.”
LNCs play a vital and advantageous role finding other experts for the case – from M.D. specialists to ancillary professionals like physical therapists, respiratory therapists, and pharmacists. Nurse expert witnesses are expected to testify at a deposition and trial if needed. Unlike the LNC consulting expert, the testifying expert may or may not be required to put their opinion in writing.
Both consulting LNCs and nurse expert witnesses review medical records and deposition testimony and formulate their conclusions. They commonly organize pertinent medical records and prepare record chronologies or timelines. They may also research medical and nursing literature and standards germane to issues in the suit brought forth. Both kinds of experts offer their own unique value to legal teams – and are often hired by healthcare organizations as risk managers or compliance experts.
As with other litigation, medical malpractice and long-term care cases often pit one expert against the other. Sometimes the tipping point in a jury’s decision is how well one witness can translate technical intricacies in to language they understand. ALN Consulting’s team of nurse consultants are in a unique position to build the strongest, most manageable court case for their clients – and boil medical-legal issues down to their essence. Contact us to learn how!
The Power of a Nurse’s Words
Wednesday, March 23rd, 2016
We here at ALN sometimes encounter a sense of “Am I making a difference and is it enough?” in our profession. And it’s interesting to hear that same thing from other nurses. Diane M Goodman recently posted a piece that so compelled us, we just had to share. Thank you, Diane.”
Sticks and Stones; The Power of a Nurse’s Words
By Diane M. Goodman, Originally appeared in MedScape, Jan 21, 2016
Many of us were raised in a generation by mothers who warned us of the old English adage about taunting others through the use of name-calling and words. We knew better. Words could either be unbelievably comforting or leave lasting scars on our memories.
As nurses, our words and our voices are no less profound. We can change the trajectory of a life by coaxing change from a desultory or despondent patient, and we can inspire peers to greatness when they feel they cannot work another moment or another busy day.
Sharing research with peers may allow them to comprehend the improbability of what we DO on a daily basis. By reading a quantitative time-study, for example, and sharing it with colleagues, they may have an improved understanding of why nurses need stress management techniques to perform their jobs. Nursing is extremely difficult work. Expecting substantive conversation or specific phrases to “just happen” at the bedside is like asking the typical pilot to land an airplane on the Hudson!
Nurses, on the average, complete >70 (!!) tasks per hour. Nurses change tasks approximately every 55 seconds. They are also interrupted approximately once every 32 minutes, with the highest amount of interruptions recorded during medication administration!*
Why is it important to know this? While this time/event study was conducted in Sydney, the research was rigorous enough to be utilized internationally as an example of why nurses may find it “difficult” to bond with patients. We may be groping to find the right words to instill initiative, hope, and change in our patients. We could even be struggling a bit.
Nina (not her real name) reminded me of this in ICU. I was struggling. She was paralyzed, intubated, ventilated, and so, so sick. I was sure she would not survive. She was only 19.
I was exhausted every night, hanging more blood, platelets and medications than I had ever hung in my life. She was septic and she had leukemia. “Sticks and stones”, I repeated in my head over and over, warning myself not to frown or sigh, or show tiredness EVER. Instead, I stroked her hair, and told her how much I loved my little sister, and my dogs. I played music for her when my voice got tired or I ran out of words. If nothing sweet or positive was left to be said, I smiled and hummed, night after exhausting night. OK, so I did a lot of humming.
Her bed was empty one night, as ICU beds often are. Rehab, they said. Long-term. Newer, sicker patients came and went.
Six months later, a young, attractive woman was wheeled in with a huge family circling her, including one very determined sister. It was Nina. She remembered nothing of her stay but a woman who stroked her hair and hummed and talked softly of dogs and family. I would have given her almost zero odds of surviving, and here she was!! Sitting tall, with very little residual effects. I couldn’t believe she remembered me! She remembered nothing else.
CMS Interpretive Guidelines – Revisions to Antipsychotic Medication Guidance
Wednesday, March 23rd, 2016
Continuing our series on the CMS Interpretive Guidelines, ALN Consulting outlines the revisions to Antipsychotic Medication Guidance. The Interpretive Guidelines include an explanation of the intent of the law, definitions of terms, and instruction on determining compliance with the law. A strong defense of long term care facility liability is grounded in an understanding of the CMS Interpretive Guidelines and its revisions. An important topic in many cases is the use of antipsychotic drugs in patient populations with dementia. This installment of our CMS series will help your team prepare for litigation involving antipsychotic medication.
The History of Antipsychotic Drug Use in Patients with Dementia
A “Black Box Warning” exists on the label of all antipsychotics reading, “Elderly patients with dementia related psychosis treated with antipsychotic drugs are at an increased risk of death. Antipsychotics are not approved for the treatment of patients with dementia related psychosis.” However, due to societal beliefs held by both families and medical providers that dementia behaviors should be treated, antipsychotic drugs have been used for some time in an “off label” way for patients with dementia. To use a drug in an “off label” manner refers to the prescription of a medication to treat a condition that has not been officially approved by the FDA for that purpose. Prescribing a drug for an “off label” reason is not illegal, and providers must use current research and standards to determine if such a use is beneficial.
Some antipsychotic use has been shown to be effective in treating symptoms of dementia, but in 2010, American Family Physician published a piece that stated, “All antipsychotic medications are associated with an increased likelihood of sedation, sexual dysfunction, postural hypotension, cardiac arrhythmia, and sudden cardiac death.” While it is not uncommon to see antipsychotics still prescribed “as needed” to control dementia behaviors, the significant risks of using antipsychotic medications in patients with dementia caused CMS to launch national partnerships and advertising to reduce off label use of antipsychotics in nursing homes in 2012.
42 C.F.R. §483.25 Quality of Care (F Tag 309)
Several regulations address the use of antipsychotic drugs in patients with dementia, and the Interpretive Guidelines were updated to reflect the most recent revisions in November 2014. The regulation for Quality of Care requires that “Residents who use antipsychotic drugs receive gradual dose reductions and behavioral interventions, unless clinically contraindicated, in an effort to discontinue these drugs.” F Tag 309 is the guidance surveyors use for review of quality of care of a resident with dementia. While there is no specific investigative protocol for care of a resident with dementia, the surveyor can use a checklist entitled, “Review of Care and Services for a Resident with Dementia.” Revisions to this Interpretive Guideline included updated definitions related to recognition and management of dementia, and specific to this topic, medication use in dementia.
The revisions in F Tag 309 to medication use in dementia stated, “When antipsychotic medications are used without an adequate rationale, or for the sole purpose of limiting or controlling behavior of an unidentified cause, there is little chance that they will be effective, and they commonly cause complications such as movement disorders, falls, hip fractures, cerebrovascular adverse events (cerebrovascular accidents and transient ischemic events) and increased risk of death.” Information and links to the FDA Black Box Warning Regarding Atypical Antipsychotics in Dementia were included. Surveyors were instructed to be on alert for antipsychotic medication administration that could be considered a chemical restraint. Specific care planning evidence should be available to show a facility included non-pharmacological approaches to dementia management, as well as gradual dose reduction of those residents on antipsychotics prescribed for dementia. Compliance and non-compliance examples were added for further clarification.
42 C.F.R. §483.25(l) Unnecessary Drugs (F Tag 329)
The regulation for unnecessary drugs also had significant revisions in November 2014. Indications for the use of antipsychotic drugs were expanded for conditions other than dementia. The F Tag 329 is designed to be used in conjunction with F tag 309 for surveyors reviewing the maintenance of behavioral or psychological symptoms of dementia patients. The new Interpretive Guideline revisions stated that antipsychotic medications are only appropriate for elderly residents in a small minority of circumstances, and “May be considered for elderly residents with dementia but only after medical, physical, functional, psychological, emotional psychiatric, social and environmental causes have been identified and addressed. Antipsychotic medications must be prescribed at the lowest possible dosage for the shortest period of time and are subject to gradual dose reduction and read review.” This revision is of special importance since many residents are admitted to long-term care already on an antipsychotic medication.
Antipsychotic medications in persons with dementia should not be used if the only indication is one or more of the following:
- wandering
- poor self-care
- restlessness
- impaired memory
- mild anxiety
- insomnia
- inattention or indifference to surroundings
- sadness or crying alone that is not related to depression or other psychiatric disorders
- fidgeting
- nervousness
- uncooperativeness (e.g., refusal of or difficulty receiving care)
All of the above highlight conditions/diagnoses where antipsychotic medications may possibly be appropriate, but diagnoses alone do not warrant the use of an antipsychotic unless the following criteria are also met:
- The behavioral symptoms present a danger to the residents or others AND one or both of the following:
- The symptoms are identified as being due to mania or psychosis OR
- Behavioral interventions have been attempted and included in the plan of care, except in an emergency
The revisions to the Interpretive Guidelines also addressed acute situations/emergencies, and enduring conditions. The guidelines include a table provided as a general guide for daily dose thresholds.
In Conclusion
Long-term care litigation requires expert knowledge in the revisions to the Interpretive Guidelines. ALN’s nursing team stands ready to guide your legal team through the changes of the key elements for Unnecessary Drug severity determination. While the updates are complex, the ALN Consulting team has the experience and expertise to build a successful defense, staying up to date with the latest revisions. Let us help you decipher the latest revisions of the Interpretive Guidelines and strengthen your long term care case.
References
- Harris, Rick E. (2015). How to Use the CMS Surveyor Guidance to Craft a Winning Defense [Presentation at the DRI LTC/SNF Seminar].
- Centers for Medicare & Medicaid Services. (2015). State Operations Manual – Appendix PP – Guidance to Surveyors for Long Term Care Facilities. Retrieved 01/04/16.
Superbugs – The Growing Problem of Antibiotic Resistant Infections
Monday, August 31st, 2015
On August 04, 2015, the Centers for Disease Control and Prevention or CDC released a report published in their monthly Vital Signs[1] newsletter regarding the increasing number of germs that no longer respond to the drugs designed to kill them. The report notes that inappropriate prescribing of antibiotics and lack of infection control actions can contribute to drug resistance and put patients at risk. Despite diligent precautions which may be implemented by one facility, these germs can be spread between health care facilities when patients are transferred from one to another.
The most common and deadliest of these superbug infections include carbapenem-resistant Enterobacteriacae or CRE which can cause deadly infections and have become resistant to nearly all antibiotics that we currently have in use. Perhaps the most commonly known antibiotic resistant infection methicillin resistant staphylococcus aureus or MRSA often causes pneumonia and sepsis. Also infections caused by Pseudomonas aeruginosa which can result in healthcare associated infection include strains that are resistant to almost all antibiotics. Clostridium difficile also known as ‘C. diff’ is a germ commonly found in health care facilities and is not resistant to antibiotics but results from antibiotic use killing the bodies “good germs” and allowing this bacterium to take over putting patients at high risk for deadly diarrhea.
In order to reduce the number of antibiotic resistant infections the CDC recommends beginning with implementation of systems to alert receiving facilities when transferring patients who have drug resistant germs as well as sharing data with the public health department about antibiotic resistance and other healthcare associated infections.
The CDC released these statistics in relation to the growing problems of antibiotic resistant infections:
- Antibiotic-resistant germs cause more than 2 million illnesses and at least 23,000 deaths each year in the US.
- Up to 70% fewer patients will get CRE over 5 years if facilities coordinate to protect patients.
- Preventing infections and improving antibiotic prescribing could avert 610,000 infections and save 37,000 lives from drug-resistant infections over 5 years. This would save the health care system nearly 8 billion dollars for treatment.
 Source: CDC Vital Signs, August 2015
Source: CDC Vital Signs, August 2015
A study cited by the CDC where researchers think a more coordinated approach may be working included the South Dakota public health department which requires health care facilities to report cases of CRE for tracking the spread of the bacteria. Infections caused by the deadly bacteria in that sparsely populated state dropped from 24 to 4 over two years. In Illinois, the state health department maintains a registry of all patients infected with drug-resistant bacteria. When a hospital or nursing home admits a patient, the facility can check the registry to see if the patient has an infection and take the appropriate precautions to prevent transmission.
At this point, infection reporting is done voluntarily and many facilities do not comply. The Centers for Medicare and Medicaid Services (CMS) has begun fining hospitals with high rates of infections and other incidents of patient harm, but those punishments are based on only a few types of bacteria.
Recommendations by the CDC for healthcare facilities to combat the spread of these antibiotic resistant infections include implementation of systems to alert receiving facilities when transferring patients who have drug-resistant germs, reviewing and improving infection control measures within their facilities, sharing data with the public health department about antibiotic resistance and other healthcare associated infections, and making sure that their clinical staff has access to prompt and accurate laboratory testing for these germs.
The agency went further making recommendations to prescribers and healthcare staff to prescribe antibiotics correctly, getting cultures then starting the right drug promptly at the right dose for the right duration, and knowing when to stop antibiotic therapy. They also recommended being aware of antibiotic resistance patterns in each facility, asking patients if they have recently received care in another facility, and most importantly following hand hygiene and other infection control measures with every patient. Patients and their families should be educated on what they can do to protect themselves and their family against these ever increasing infections including informing health care workers if they have been hospitalized in another facility and insisting that everyone wash their hands before touching them as well as washing their own hands often.
Dr. John Jernigan, an official with the CDC and senior author of the paper stated, “Facilities can’t do it alone. There are not many places where a coordinated effort is happening and we think we need to do a much better job.”
[1] http://www.cdc.gov/vitalsigns/stop-spread/
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm64e0804a1.htm?s_cid=mm64e0804a1_w