CMS Interpretive Guidelines – Revision to Feeding Tube Guidance
In this installment of the ALN Consulting series on the CMS Interpretive Guidelines, we explore the most recent revisions to surveyor guidance on feeding tubes in long-term care facilities. The Interpretive Guidelines include an explanation of the intent of the law, definitions of related terms, and instructions to surveyors on how to determine compliance with the law.
The CMS Interpretive Guidelines for Nasogastric tubes updates clarify expectations for long-term facility accountability in regards to use of feeding tubes; requiring that the resident’s legal representative be properly informed, specifying how nutritional needs are monitored, and mandating that potential risks associated with feeding tubes be considered in the decision making process.
The key to a strong defense against complaints related to long-term care residents’ nutritional status, particularly those who have feeding tubes, lies in a solid understanding of these guidelines and the recent revisions.
42 C.F.R. §483.25(g) Nasogastric Tubes (F tag 322)
The CFR Regulation states, “Based on the comprehensive assessment of a resident, the facility must ensure that:
- A resident who has been able to eat enough alone or with assistance is not fed by nasogastric tube unless the resident’s clinical condition demonstrates that use of a nasogastric tube was unavoidable; and
- A resident who is fed by a nasogastric or gastrostomy tube receives the appropriate treatment and services to prevent aspiration pneumonia, diarrhea, vomiting, dehydration, metabolic abnormalities, and nasal-pharyngeal ulcers and to restore, if possible, normal eating skills.”
Relevant definitions in the Interpretive Guidelines include:
Avoidable: There is not a clear indication for using a feeding tube, or there is insufficient evidence it provides a benefit that outweighs associated risks.
Unavoidable: There is a clear indication for using a feeding tube, or there is sufficient evidence it provides a benefit that outweighs associated risks.
Bolus feeding: The administration of a limited volume of enteral formula over brief periods of time.
Continuous feeding: The uninterrupted administration of enteral formula over extended periods of time.
Enteral nutrition (a.k.a. “tube feeding”): The delivery of nutrients through a feeding tube directly into the stomach, duodenum, or jejunum.
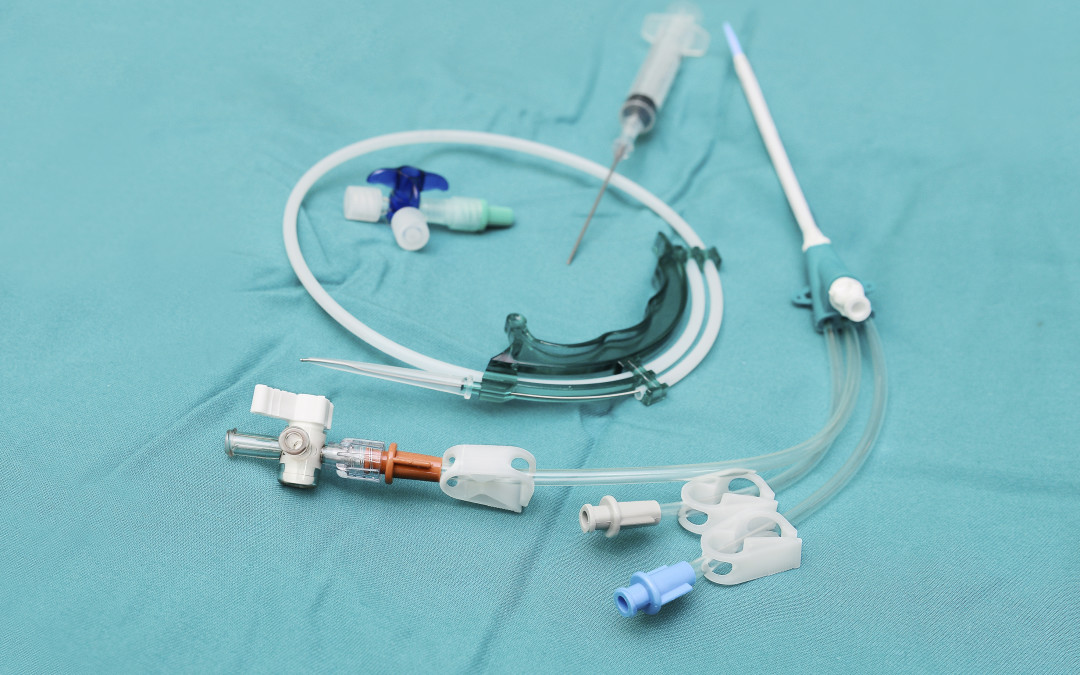
Feeding tube: A medical device used to provide enteral nutrition to a resident by bypassing oral intake.
Gastrostomy tube (“G-tube”): A tube that is placed directly into the stomach through an abdominal wall incision for administration of food, fluids, and medications. The most common type is a percutaneous endoscopic gastrostomy (PEG) tube.
Jejunostomy tube (a.k.a. “percutaneous endoscopic jejunostomy” (PEJ) or “J-tube”): A feeding tube placed directly into the small intestine.
Nasogastric feeding tube (“NG tube”): A tube that is passed through the nose and down through the nasopharynx and esophagus into the stomach.
Transgastric jejunal feeding tube (“G-J tube”): A feeding tube that is placed through the stomach into the jejunum and that has dual ports to access both the stomach and the small intestine.
Tube feeding (a.k.a. “enteral feeding”): The delivery of nutrients through a feeding tube directly into the stomach, duodenum, or jejunum.
Regulation Tag F 322
The feeding tube requirement has two parts. The first aspect requires that the facility utilize a feeding tube only after it determines that a resident’s clinical condition demonstrates this intervention was unavoidable. The second aspect requires that the facility provides to the resident who is fed by a tube services to prevent complications, to the extent possible, and services to restore normal eating skills, if possible.
The facility is in compliance with 42 CFR §483.25(g), if staff:
- Uses a feeding tube to provide nutrition and hydration only when the resident’s clinical condition makes this intervention necessary based on adequate assessment, and after other efforts to maintain or improve the resident’s nutritional status have failed;
- Manages all aspects of a feeding tube and enteral feeding consistent with current clinical standards of practice in order to meet the resident’s nutritional and hydration needs and prevent complications; and
- Identifies and addresses the potential risks and/or complications associated with feeding tubes, and provide treatment and services to restore, if possible, adequate oral intake.
Surveyor “Probes” in Facility Use of Feeding Tubes
Probes, or questions posed by the Interpretive Guidelines for surveyors, can be used by the defense team to bolster evidence that a practitioner or facility met the standard of care. There are many probes in F tag 322 related to resident rights; technical and nutritional aspects of feeding tubes; care of the feeding tube; and complications related to the feeding tube and/or the enteral nutrition product. Some examples of surveyor probes include:
- Was the resident and/or the resident’s legal representative informed about the relevant benefits and risks of tube feeding?
- How has the staff and practitioner determined the cause of decreased oral intake/weight loss or impaired nutrition and attempted to maintain oral intake prior to the insertion of a feeding tube?
- How did the staff determine the resident’s nutritional status was being met, such as periodically weighing the resident, and how did they decide whether the tube feeding was adequate to maintain acceptable nutrition parameters?
- How has the facility identified the resident at risk for impaired nutrition, identified and addressed causes of impaired nutrition, and determined that use of a feeding tube was unavoidable?
- How has the staff verified that the feeding tube was properly placed?
- How has the staff monitored a resident for possible complications (e.g., diarrhea, nutritional deficits, aspiration, depression, withdrawal, etc.) related to a feeding tube and the tube feeding, and how have they identified and addressed such complications?
Updates to the Interpretive Guidelines
The Interpretive Guidelines entitled Nasogastric tubes was vastly updated in November 2014. For the purpose of the guidelines, the regulatory title is considered to include any feeding tube used to provide enteral nutrition to a resident by bypassing oral intake. (Since the regulation was created use of actual nasogastric tubes have become rare, and use of other types of enteral feeding tubes have become more prominent.)
The newest guidance stresses the unavoidability standard, and also emphasizes quality of life and resident choice. Based on the guidelines, it could be argued that some examples of possible adverse effects from feeding tubes such as diminished socialization and loss of the experience of taste, texture, and chewing must be considered as important, and may possibly outweigh the benefits of feeding tubes such as preventing malnutrition and dehydration, and aiding wound healing. A new statement regarding the use of feeding tubes in elderly patients with dementia also addressed the controversy in this arena. “The literature regarding enteral feeding of these individuals suggests that there is little evidence that enteral feeding improves clinical outcomes (e.g., prevents aspiration or reduces mortality).”3
In the defense of the use, non-use, or complications of feeding tubes, the Interpretive Guidelines; Nasogastric tubes now provide a much larger framework for the difficult end of life decisions which are inherent in turning towards non-oral sustenance. With the comprehensive updates added to this guideline, ALN Consulting can help your defense team pinpoint crucial, relevant prompts and research to strengthen a case with complaints involving tube feeding.
References
- Harris, Rick E. (2015). How to Use the CMS Surveyor Guidance to Craft a Winning Defense [Presentation at the DRI LTC/SNF Seminar].
- Centers for Medicare & Medicaid Services. (2015). State Operations Manual – Appendix PP – Guidance to Surveyors for Long-term Care Facilities. Retrieved 02/23/16.
- Compliance Solutions for the Perfect Survey Every Day. (2014). F322. Retrieved 02/23/16 from The Perfect Survey website.