Liability Risks Could Be Linked To Staffing Shortages

Staffing shortages can cause a wide range of problems within a healthcare facility. Literature shows that understaffing is directly related to physical exhaustion and burnout, which can lead to poor judgment, accidents, safety concerns, and increased mistakes. These issues can lead to more significant liability risks, including professional liability, general liability, and workers’ compensation claims. Risk managers are struggling to alleviate those risks even as the staffing challenges do not look good in the near future. Recent research indicates nurse staffing is near crisis levels, with fewer than one-quarter of nurses saying their facilities are adequately staffed at least 75% of the time.
Contributing factors impacting the nursing shortage include:
• Nursing school enrollment is not growing fast enough to meet the projected nurse demand.
• A shortage of nursing school faculty is restricting nursing program enrollments.
• A significant segment of the nursing workforce is nearing retirement age.
• Changing demographics signal a need for more nurses to care for our aging population.
• Amplified by the pandemic, insufficient staffing is raising the stress level of nurses, impacting job satisfaction, and driving many nurses to leave the profession.
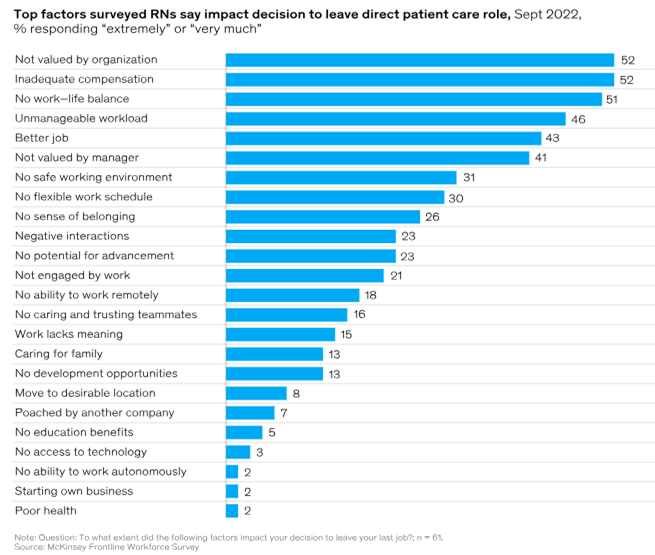
According to a McKinsey Frontline Workforce Survey:
According to the Bureau of Labor Statistics Employment Projections 2021-2031, the Registered Nursing (RN) workforce is expected to grow by 6% over the next decade, from 3.1 million in 2021 to 3.3 million in 2031, an increase of 195,400 nurses. The Bureau also projects 203,200 openings for RNs annually through 2031, when nurse retirements and workforce exits are factored into the number of nurses needed in the U.S.
As staffing shortages persist, risks continue to trickle down to patients, and this can be seen through the quality of care, including hospital-acquired conditions (HACs), the inability to complete daily necessary care tasks, missed medications, and safety issues. It is imperative for healthcare organizations to look at short-term and long-term approaches to staffing shortages, including working with local nursing schools on partnerships and internships, benefits packages, and considering alternative scheduling and patient care models. Organizations should maximize electronic health records and other clinical technology to reduce unnecessary actions by nursing and other staff. Administrative and repetitive tasks should be automated to reserve more time for staff to interact with patients. Using job flexibility strategies to attract new talent and welcome back nurses who left during the pandemic is one way to decrease an organization’s staffing shortages. Henry Ford Health returned 25 percent of the nurses who left by offering flexible opportunities. Flexible options included things such as the ability to work in different settings (for example, inpatient, outpatient, or virtual) or to work only on weekends. The health system also created fixed-term positions for nurses who didn’t want full-time permanent jobs, with the option once their term was up.
As staffing shortages persist, there will likely be a link between hospital staffing shortages and increased claims from liability and workers’ compensation standpoints. Med Law Advisory Partners has the expertise to review all aspects of hospital and long-term care facility cases to determine if the standards of care were met. Contact us today to add our expertise to your team.