National Pressure Ulcer Advisory Panel (NPUAP) Release New Clinical Guidelines and Taxonomy for Pressure Injuries

In 1986, the National Pressure Ulcer Advisory Panel (NPUAP) was formed as an independent, non-profit organization established to ensure consistent prevention, management and research of pressure ulcers. Conflicts in research and prevention created the need for this governing body, an organization that would work to create guidelines and establish best practices surrounding pressure injury wounds. NPUAP serves as the authoritative voice for improved patient outcomes in pressure ulcer prevention and treatment through the development of public policy, education and research.
Subsequent to the formation of NPUAP, the terminology to describe “pressure ulcers” was redefined and the staging system of pressure wounds expanded. Although changes were made with the intent of clarifying the differences among the stages of pressure ulcers, the new classification system led to more confusion. For example, the use of the term “injury” and “ulcer” interchangeably caused great confusion.
In April 2016, a consensus conference was convened by NPUAP to review and revise the pressure injury staging system and to standardize the terminology used to describe injury to the skin from external pressure. The term “pressure ulcer” was changed to “pressure injury.” This simple change in terminology was actually monumental, as it was a major departure from the old taxonomy in the 30 years since the panel was formed. Updates to the panel’s description of the stages of pressure injuries were developed. The group indicated that the change in terminology would more accurately describe pressure injuries to both intact and ulcerated skin.
The 2016 definition of “Pressure injury” by NPUAP describes localized damage to the skin and underlying soft tissue usually over a bony prominence, related to a medical procedure such as prolonged surgery or from a medical device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shearing forces. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue. Shearing occurs from friction against the skin that leads to a superficial or partial thickness injury, often resembling an abrasion.
Pressure Injury Staging
The staging system further defined pressure injuries of stages 1-4 as well as including medical device related pressure injuries and mucosal membrane pressure injuries. The following illustrations denote each stage and classification of pressure injuries.
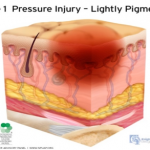 Stage 1 Pressure Injury: Non-blanchable erythema of intact skin. Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple of maroon discoloration; these may indicate deep pressure injury.
Stage 1 Pressure Injury: Non-blanchable erythema of intact skin. Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple of maroon discoloration; these may indicate deep pressure injury.
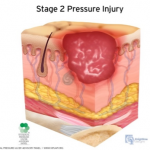 Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible nor are deeper tissues. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible nor are deeper tissues. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
Stage 3 Pressure Injury: Full-thickness skin loss. Full thickness loss of skin, in which adipose tissue is visible in the ulcer, meets the definition of a Stage 3 pressure injury. Granulation tissue and epibole (rolled wound edges) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss, this becomes an Unstageable Pressure Injury.
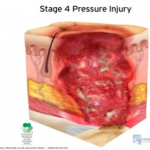 Stage 4 Pressure Injury: Full-thickness skin and tissue loss. Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole, undermining and/or tunneling often occur. The depth of the injury varies by anatomical location. If slough or eschar obscures the extent of tissue loss, an injury such as this would be described as an Unstageable Pressure Injury.
Stage 4 Pressure Injury: Full-thickness skin and tissue loss. Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole, undermining and/or tunneling often occur. The depth of the injury varies by anatomical location. If slough or eschar obscures the extent of tissue loss, an injury such as this would be described as an Unstageable Pressure Injury.
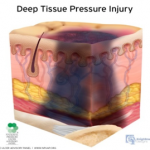 Deep Tissue Pressure Injury: persistent non-blanchable deep red, maroon or purple discoloration. This type of injury may involve either intact or non-intact skin, presenting with a localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss.
Deep Tissue Pressure Injury: persistent non-blanchable deep red, maroon or purple discoloration. This type of injury may involve either intact or non-intact skin, presenting with a localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss.
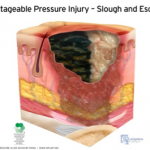
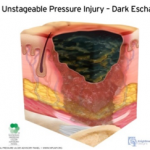 Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss. This type of injury involves full-thickness skin and tissue loss. The extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If the slough or eschar is removed from the wound, a stage 3 or stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss. This type of injury involves full-thickness skin and tissue loss. The extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If the slough or eschar is removed from the wound, a stage 3 or stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
As classifications and guidelines change, it’s critical to have an expert on your team who understands the current definitions. ALN Consulting’s team of legal nurse consultants have their finger on the pulse of these changes, and are trained to spot inaccuracies in medical records that can effect case outcomes. Contact ALN Consulting today to learn how we can help.
