The Law and the Glasgow Coma Scale
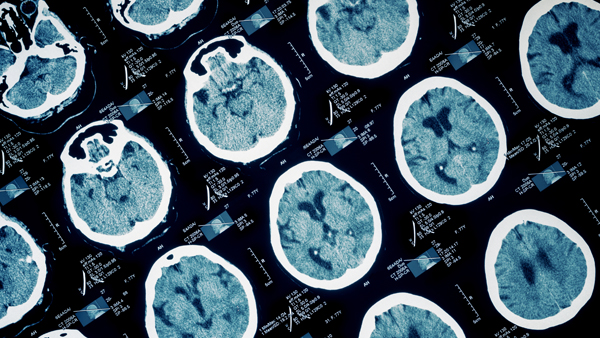
When pursuing legal action for clients who have sustained a traumatic brain injury (TBI), attorneys must be able to assess the progression of damage and the prognosis for recovery. One of the first steps is understanding the most common scoring system used to describe and record levels of consciousness in persons with an acute brain injury. Known as the Glasgow Coma Scale (GCS), the scale is a practical method of assessing impaired conscious level in persons injured from any cause, although it is most frequently used in cases of head injury.
First described in 1974 by neurosurgeons at the University of Glasgow, Scotland, the GCS was developed to provide a “universal” method of describing the responsiveness of a patient in simple, objective terms. The verbiage has evolved since its introduction, but the scale itself has largely remained the same over time. It has become a critical tool for first responders, paramedics, and emergency room staff for measuring the degree of an acute brain injury.
The GCS measures functions involving eye opening, verbal response, and motor response. On a scale ranging between 3 and 15, a score below 8 indicates a severe injury, while 13 and above is considered a mild impairment. Clinicians use this scale to rate the best eye opening response, the best verbal response, and the best motor response an individual makes. The final GCS score is the sum of the number points in those categories. A modified version of the GCS is the Pediatric Glasgow Coma Scale (PGCS) which considers the eye, verbal, and motor response tests separately as well together.
This scoring system guides initial medical decisions and monitors changes in responsiveness. It is useful in monitoring chronic patients in intensive care. But even out of the ICU, the scale helps nurses spot important changes in a patient’s condition. The timing and frequency of the assessment is individualized. The role of the scale is to support and not replace clinical decision making.
Measuring Traumatic Brain Injury Response
The adult Glasgow Coma Scale measures functions as follows:
Eye Opening (E)
- 4 – Spontaneous
- 3 – In response to voice
- 2 – In response to pain
- 1 – None
Verbal Response (V)
- 5 – Normal conversation
- 4 – Disoriented conversation
- 3 – Incoherent words
- 2 – No words, only sounds
- 1 – None
Motor Response (M)
- 6 – Normal
- 5 – Localized to pain
- 4 – Withdraws to pain
- 3 – Decorticate posture (an abnormal posture that can include rigidity, clenched fists, legs held straight out, and arms bent inward toward the body with the wrists and fingers bend and held on the chest)
- 2 – Decerebrate posture (an abnormal posture which can include rigidity, arms and legs held straight out, toes pointing downward, head and neck arched backwards)
- 1 – None
The Glasgow Coma Scale is not without its limitations. It only indicates a conscious level at the time the test is administered. By itself, it does not reveal how long someone has been unconscious or even, in the case of a high score, that he or she was unconscious at all at a previous point. A dead patient can still be assigned a GCS of 3.
Some researchers are concerned with the GCS’s poor inter-rater reliability, or degree of agreement or consensus among those assessing a patient’s condition. It can also limited by the training a first responder or paramedic has in identifying and assessing brain injury.
A measurable level of brain injury can fluctuate significantly over minutes or hours – especially considering factors like shock, low blood oxygen, and the presence of drugs or alcohol in a patient’s system. A GCS score can obviously improve by the time the patient reaches the emergency room. A very low score does not mean that a patient will never recover from his or her TBI. Likewise, a very high score does not mean that there is no brain injury present. The Glasgow Coma Scale complements, rather than substitutes, other neurological assessments.
When an accident involves a traumatic brain injury, time can be as valuable a resource as money for plaintiffs, defendants, and attorneys alike. Explicating all the fine points of consciousness and TBI takes plenty of both. A legal nurse consultant reviews client medical records and independently investigates the case. Your LNC can help your legal team determine a case’s merit and efficiently pinpoint medical issues and other factors that will affect how you proceed.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.