Archive for the ‘Blog’ Category
Liability Risks Could Be Linked To Staffing Shortages
Tuesday, September 19th, 2023
Staffing shortages can cause a wide range of problems within a healthcare facility. Literature shows that understaffing is directly related to physical exhaustion and burnout, which can lead to poor judgment, accidents, safety concerns, and increased mistakes. These issues can lead to more significant liability risks, including professional liability, general liability, and workers’ compensation claims. Risk managers are struggling to alleviate those risks even as the staffing challenges do not look good in the near future. Recent research indicates nurse staffing is near crisis levels, with fewer than one-quarter of nurses saying their facilities are adequately staffed at least 75% of the time.
Contributing factors impacting the nursing shortage include:
• Nursing school enrollment is not growing fast enough to meet the projected nurse demand.
• A shortage of nursing school faculty is restricting nursing program enrollments.
• A significant segment of the nursing workforce is nearing retirement age.
• Changing demographics signal a need for more nurses to care for our aging population.
• Amplified by the pandemic, insufficient staffing is raising the stress level of nurses, impacting job satisfaction, and driving many nurses to leave the profession.
According to a McKinsey Frontline Workforce Survey:
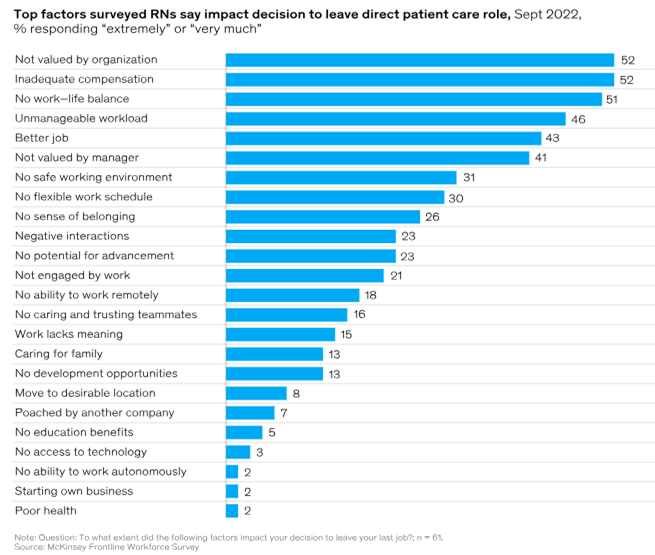
According to the Bureau of Labor Statistics Employment Projections 2021-2031, the Registered Nursing (RN) workforce is expected to grow by 6% over the next decade, from 3.1 million in 2021 to 3.3 million in 2031, an increase of 195,400 nurses. The Bureau also projects 203,200 openings for RNs annually through 2031, when nurse retirements and workforce exits are factored into the number of nurses needed in the U.S.
As staffing shortages persist, risks continue to trickle down to patients, and this can be seen through the quality of care, including hospital-acquired conditions (HACs), the inability to complete daily necessary care tasks, missed medications, and safety issues. It is imperative for healthcare organizations to look at short-term and long-term approaches to staffing shortages, including working with local nursing schools on partnerships and internships, benefits packages, and considering alternative scheduling and patient care models. Organizations should maximize electronic health records and other clinical technology to reduce unnecessary actions by nursing and other staff. Administrative and repetitive tasks should be automated to reserve more time for staff to interact with patients. Using job flexibility strategies to attract new talent and welcome back nurses who left during the pandemic is one way to decrease an organization’s staffing shortages. Henry Ford Health returned 25 percent of the nurses who left by offering flexible opportunities. Flexible options included things such as the ability to work in different settings (for example, inpatient, outpatient, or virtual) or to work only on weekends. The health system also created fixed-term positions for nurses who didn’t want full-time permanent jobs, with the option once their term was up.
As staffing shortages persist, there will likely be a link between hospital staffing shortages and increased claims from liability and workers’ compensation standpoints. Med Law Advisory Partners has the expertise to review all aspects of hospital and long-term care facility cases to determine if the standards of care were met. Contact us today to add our expertise to your team.
Long-Term Care: Are Your Residents at Risk?
Tuesday, August 22nd, 2023
Resident safety and welfare in long-term care (LTC) is being redefined as the focus shifts to promoting an optimal quality of life. Achieving this requires applying knowledge of best practices for identifying, communicating, documenting, and managing the risks that arise from the choices made in the pursuit of a better quality of life. Proactive risk management requires identifying the hazards associated with a resident’s choices and implementing interventions to enhance their quality of life.
The first step in preventing adverse events during a residency in a long-term care facility includes determining risk, whether it is a risk for falls, infections, nutritional deficits, pressure injuries, or any adverse event. Upon completion of risk assessments, the risk factors identified should guide you in developing a care plan. Preventative measures should be implemented, and the effectiveness of those interventions should be evaluated based on the individual resident’s risk factors and goals.
Falls are the leading cause of death in adults aged 65 or older. Regulations set forth by the Centers for Medicare and Medicaid Services (CMS) include F-Tag 689 regarding accidents. This regulation includes assessing the individual resident’s risk for an accident. Generally, this can be accomplished using a fall risk assessment which should be performed on admission and at least quarterly after that. Multiple fall risk assessment tools are available for use and can provide the needed risk determination. These may include but are not limited to the Morse Falls Scale, the Briggs Healthcare Fall Risk Assessment, and the Hendrich II Fall Risk Model. An accurate assessment of a resident’s risk for falls and accidents will ensure compliance with CMS regulations and initiate the pathway for fall/accident prevention.
The current standard of care in pressure injury prevention is based on risk assessment and visual assessment of skin in areas prone to pressure injuries. Per the Centers for CMS F-Tag F686 for the prevention of pressure injuries, the facility must first identify whether the resident is at risk for developing or has a pressure injury upon admission. To prevent a resident from developing a pressure injury, their risk factors should be determined via the comprehensive resident assessment. A formal risk assessment tool is an excellent way to identify some – but not all – risk factors. Such tools can include a Braden Scale and the Norton Plus Pressure Ulcer Scale. Current recommendations indicate that the assessments should be performed on initial admission, weekly for four weeks, and quarterly after that and as needed. Assessments should also be performed on re-admission to the facility following a stay in the hospital or an outside facility.
Dehydration is common in the elderly and a frequent cause of hospital admission. CMS Regulation F-Tag F692 regarding assisted nutrition and hydration includes recognizing the needs of every resident concerning their risk for impaired nutrition and hydration. Again, an initial accurate assessment of a newly admitted resident’s risk for these impairments is paramount to ensure these issues are avoided if possible. A malnutrition risk assessment can be beneficial in determining this risk.
The importance of accurately determining those residents at risk for adverse events cannot be overstated. The Med Law Advisory Partners team are experts in regulations affecting long-term care facilities and providing guidance if or when adverse events occur. Contact us today to add our expertise to your arsenal.
Meaningful Use of Metadata in Medico-Legal Case Review
Tuesday, July 11th, 2023
In the past, medical records were written on paper, subject to its associated disadvantages, including the ability to easily change and destroy physical paperwork. Now, medical records are “written” electronically and maintained and retrieved digitally in electronic health records (EHRs). These EHRs contain not only the printed health records but trails of the data entered and hardware and software safeguards in place to prevent manipulation.
With the advent of electronic health records, the information relevant to medical malpractice case reviews is not just included in the patient record. There exist complex trails of information which tell the story of each entry into the electronic health record, including how it was entered, when, and by whom. While the information in the medical record is considered data, the contextual information that helps us understand what that data is, its evolution and all of its iterations over time is metadata.
Essentially, metadata is background explanatory information that tells the digital data story. The metadata details reveal the underlying data’s source, type, owner, and relationships to other data sets in the records. In the case of medical record entries, metadata can reveal precisely when chart entries occurred, who made them, if they were viewed, by whom, and if they were removed or revised, including all versions. Without metadata, the history of electronic data is unknown.
Generally, there are three types of metadata: descriptive, administrative, and structural – but all types, in some critical manner, tell the digital data’s story. The information generated and stored by computer applications, including electronic health record platforms, is complex. Nevertheless, it is extremely important to fully evaluate patient records for medico-legal purposes. The importance of audit trails in electronic health records, thus, cannot be overstated since they may hold the key to evidence of altered records, proof of timing, and other critical information vital to a litigant’s position. The same holds true for computerized information when we looked at evidence of rewritten notes and added or deleted entries. While the data is more complex, the concept remains the same. When analyzing medical records, we must be savvy enough to identify how metadata may be analyzed to support or refute specific allegations. The metadata generated by electronic health record software platforms provides information regarding access and modifications of a specific patient’s electronic health record.
What you see in the printed, electronic health record is not the entirety of the medical record. If you access the metadata and you can determine when data was entered, modified, accessed, or printed, you then have much more information than just what is in the viewable record received in a file or printed. Pieces of the puzzle can be extrapolated from that information based on professional evaluation and practice expertise. The metadata is critical information that Med Law’s team is experienced in reviewing, evaluating, and, most importantly, critically linking to meaningful supporting evidence. Let us discuss with you how metadata may be a critical aspect of case review you may be overlooking.
The Growth of Telemedicine: Advantages and Dangers
Thursday, June 29th, 2023
Telemedicine uses technology to deliver medical care from a healthcare provider to a patient in a different location. While telemedicine services are not necessarily new in healthcare, their use has suddenly expanded with the Covid-19 pandemic.
Telemedicine was already growing in popularity before the Covid-19 pandemic. By 2018, the American Medical Association said more than 25% of U.S. physicians worked in a practice that used telemedicine. But, pandemic-related changes gave telemedicine a big boost. Most significantly, the percentage of medical practices using video conferencing with patients increased from 14.3% in 2018 to 70.3% in 2020.
One study of the use of telemedicine visits versus in-person appointments during the last three months before the pandemic and the first three months of the pandemic showed that after mid-March 2020:
- Young adults were more than 22 times as likely to use telemedicine after the pandemic started than they had been previously
- Children and teens were more than 58 times as likely to use telemedicine after mid-March 2020
- People aged 65 and older were 237 times as likely to rely on telemedicine visits after the pandemic got underway
At Ohio State’s Wexner Medical Center, telemedicine visits jumped from 96 in February 2020 to 202,900 between March and July of the same year.
With an increase in this type of health care comes the risk of associated litigation. Medical providers must note that most of the same legal pitfalls of clinical practice are also present in a telemedicine practice, including the need for careful compliance with federal and state regulations. There have been relatively few medical malpractice claims associated with telemedicine visits, mainly because the most common contexts for medical malpractice claims are not addressed through telemedicine, such as surgical errors. However, some potential types of malpractice that can and do happen in telemedicine settings are misdiagnosis, failure to diagnose or delayed diagnosis, and prescription medication errors. When these and other errors occur due to a healthcare provider’s negligence, the injured patient’s rights and options are very much the same as if the negligence had happened in an in-person visit.
As important as it is for a physician to understand the limitations of telemedicine, it is equally important for their patients to understand their limitations. Physicians should make it clear to their patients that telemedicine can be used in a limited number of circumstances as it limits the ability of a physician to examine the patient physically. If patients expect too much from a physician, they will be let down when their expectations are not met, and that disappointment can lead to a lawsuit. When patients are well informed about the limitations of telemedicine, they will be less likely to expect a physician to provide the same services to them in a virtual setting as they could at an in-person office visit.
For a plaintiff to make a case for medical malpractice, they must prove that a physician breached the standard of care. A common definition of the standard of care is what a reasonable physician of similar education, training, and experience would have done in the same or similar circumstances. This means the standard of care could differ for an in-person office visit versus a telemedicine visit. However, it is anticipated that plaintiff attorneys will argue that both standards of care should be the same.
This new technology, as is the standard of care applied to telemedicine, is rapidly evolving. It is anticipated that there will be an increase in litigation stemming from telemedicine due to its rise in usage and the impersonal nature of the platform. Physicians should be cautious of the limitations of the technology, keep their patients informed, and document well. There are many advantages to telemedicine due to its inherent convenience and ability to record segments of the discussions. The rapid rate of adoption of telemedicine is likely to continue, and in turn, it will produce its own body of law.
At Med Law Advisory Partners, we evaluate medical malpractice claims and assist our clients by completing thorough medical record reviews and analyses for breaches in standards of care. Let us help you not only when litigation arises but let us help you identify potential issues upstream to avoid litigation downstream.
Be Prepared to Defend a Choking Incident in Long-Term Care or Assisted Living Settings
Monday, May 15th, 2023
Choking is the fourth leading cause of unintentional injury death in the United States. In 2021, there were approximately 5,325 choking deaths in the United States. Statistics show that the overall instances of choking are gradually increasing and are most prevalent among the elderly, with food most often responsible for such incidents. This increased risk in the elderly is partly due to risk factors, including age-related changes, the use of dentures, living alone, medications, and difficulty swallowing. Dysphagia, or difficulty swallowing, is a significant risk factor for choking at any age. However, chronic diseases which often affect the elderly population, including cerebrovascular disease, Parkinson’s disease, Alzheimer’s disease, or dementia, increase the risk of developing dysphagia and therefore increase the risk of choking. Since the cough reflex has motor, sensory, and cognitive components, this reflex decreases with age, increasing the risk of choking and aspiration in the elderly. Additionally, the need for medication with sedative qualities, such as antipsychotics, opioid analgesics, hypnotics, and anti-anxiety medications, impact the central nervous system and can also impair the integrity of the swallow and cough reflexes, increasing the risk of choking.
Can choking be prevented?
Although not all choking events can be prevented, the first line of defense in preventing any potential issue/incident is risk assessment. Residents of long-term care and assisted living facilities should be screened on admission for any difficulties with chewing or swallowing. This is often done as a part of the admission assessment by the nursing staff and during nutritional assessments, allowing for early recognition and intervention. The following features may help to identify elders at risk of eating or swallowing problems;
1. Increased age (more than 65 years of age)
2. Poor dental status
3. Postural instability during meals
4. Poor mobility
5. Fatigue during meals
6. Sedative, opioid, or antipsychotic medications
7. Chronic vs. acute lung infections
8. Diagnoses associated with possible dysphagia
A multidisciplinary approach in the assessment of each resident is of utmost importance. Should issues with swallowing be identified, speech therapy should be involved for additional assessments and treatment. More specific swallowing assessments may be utilized, including fiberoptic endoscopy of swallowing (FEES) or videofluoroscopy (VFS). Based on assessment findings, multiple methods can be used to prevent choking in those deemed at risk. Interventions can include texture modification of foods, ensuring proper positioning during intake, implementation of swallowing maneuvers, provision of thickened liquids, alternating intake of foods and fluids during meals, providing assistance with intake, and supervision. The importance of supervision of the elderly during meal times cannot be overstated. Additionally, residents who have dementia and/or wander and may pick up food from other sources while unattended are at risk for choking in a long-term care or assisted living facility setting and would require additional supervision. Staff education and training concerning providing food and snacks as ordered by the physician and the ability to perform first aid should a choking episode occur is also paramount.
The legal nurse consultants of Med Law Advisory Partners are well-versed in the standards of care and regulations governing long-term care and assisted living facilities throughout the nation. We at Med Law Advisory Partners can assist with the defense of these cases and help you to reduce facility liability.
Outdated Healthcare Staffing Models Silently Thwart Risk Management Goals
Thursday, April 20th, 2023
Recent significant strains on our healthcare system, especially bedside care providers, have highlighted the reality that institutional staffing ratios currently employed are based on outdated care delivery models and unrealistic budgetary considerations. As a result, organizational leadership is continually tasked with staffing units for maximum patient outcomes while exhausting the least resources possible. Historically, formulas have determined patient care staffing needs by calculating hours per patient per day. While individual state legislation has improved transparency in staffing ratios, the impact on actual patient care has been less than seismic. Continued focus on numbers rather than acuity and nurse skill level have plagued the process, and while staff has certainly suffered, patients have borne the brunt of this system failure.
From a risk management perspective, the trajectory from insufficient staffing to poor care and less-than-optimal outcomes should not be a surprise. Yet, somehow, to many facility executives, it is. Current evidence-based research points to lower nurse-to-patient staffing ratios as a key quality indicator for disease-specific outcomes and patient satisfaction. According to the American Nurses Association, we continue to face a staffing crisis challenged by an aging population, cost-saving strategies, and workplace stressors. Sicker patients with complex, multifaceted, interdisciplinary needs are the rule rather than the exception. Staffing models that consider the acuity of patients and the number of patients, while seemingly obvious, are rarely utilized.
Day after day, nurse staffing ratios continue to be purely numbers-driven. Even as the Covid pandemic magnified how patient acuity influences staffing deficiencies, numbers continued to drive staffing, fueling staff burnout and compassion fatigue, dissatisfied patients and families, and unsafe delivery of care. Nurse staffing norms are pennywise but pound foolish, adding to increased areas of exposure to liability requiring countless dollars spent defending resultant negligence claims. A thorough evaluation of how staffing is determined, considering more than just dollars and cents, but the complexity of patient acuity, nurse skill level, presence of ancillary staff, and treatments ordered, while more expensive, is more cost-effective in the long run.
The future of patient care delivery must include staffing ratios that allow for the realistic achievement of safe, evidence-based, quality care. Cost-prohibitive staffing ratios simply cannot support long-term risk management goals. Finding a way to fund more liberal staffing measures is a key component to achieving a culture of safety that respects the staff as human beings rather than numbers. Shifting away from numbers-based staffing is how leaders can chip away at the perils of poor patient outcomes while streamlining costs. Don’t get caught in the loop of endless tail chasing, trying to meet unworkable staffing expectations. Instead of ignoring patient acuity, incorporate it into your staffing model. The result will likely be long-term cost savings through decreased exposure to the liability pitfalls inherent in unreasonable staffing constraints.
At Med Law Advisory Partners, we not only evaluate medical malpractice claims but also assist our clients by looking for patterns of gaps in care that may indicate insufficient staffing, exposing the facility to litigation. Let us help you not only when litigation arises but let us help you identify potential issues upstream to avoid litigation downstream.
Hospital Discharge to Home Versus a Skilled Nursing Facility
Thursday, March 30th, 2023
Since the introduction of the prospective payment system (PPS), hospitals have had a financial incentive to discharge patients quickly because Medicare, for the most part, pays a fixed rate for hospitalizations without regard to the length of stay. Many discharge planners view their roles as cost control. When the discharge is not to a skilled nursing home (SNF), follow-up for unresolved medical problems is critical. Post-hospital acuity levels have increased, resulting in more complex arrangements and increased teaching needs for patients and family caregivers.
To facilitate an appropriate discharge from the hospital, The Center for Medicare and Medicaid Services has the following regulation in effect:
• 42 CFR § 482.43 – Condition of participation: Discharge planning. The hospital must have an effective discharge planning process that focuses on the patient’s goals and treatment preferences and includes the patient and his or her caregivers/support person(s) as active partners in the discharge planning for post-discharge care. The discharge planning process and the discharge plan must be consistent with the patient’s goals for care and his or her treatment preferences, ensure an effective transition of the patient from hospital to post-discharge care, and reduce the factors leading to preventable hospital readmissions.
A study investigating the association of patient outcomes and Medicare costs of discharge home with home health care vs. discharge to a skilled nursing facility was conducted using more than 17 million hospitalizations from January 1, 2010, through December 31, 2016. 38.8% were discharged home with home health, and 61.2% were discharged to a skilled nursing facility (SNF). The patients discharged home experienced a 5.6 % higher readmission rate at 30 days than those discharged to the SNF. However, there were no significant differences in 30-day mortality rates or improved functional status. Medicare payments for those discharged home for post-acute care were significantly lower than those discharged to an SNF.
Skilled nursing facilities consistently received a higher share of hospital discharges compared to home healthcare agencies towards the last quarter of 2021 and the beginning of the first quarter of 2022, a shift from the home health trend in the early days of the pandemic. However, signs suggest home health referrals are much higher overall than before the pandemic. Even if demand for home health services is increasing, the demand for agencies’ bottom lines is based on staffing capacity. In January 2022, the home care industry’s referral rejection rate had reached 58%, according to Tom Martin, director of post-acute care analytics at WellSky. “This is telling us that [providers] can’t take this high volume of patients looking for home health services, and they’re starting to turn down more and more patients from their referral partners.
While increasing disease burden and rising healthcare costs in the United States have already contributed to a boost in care at home services, the COVID-19 pandemic has created a catalyst to reimagine their future. It is estimated that up to $265 billion worth of care services (representing up to 25 percent of the total cost of care) for Medicare FFS (fee for service) and MA (Medicare Advantage) beneficiaries could shift from traditional facilities to the home by 2025 without a reduction in quality or access. Factors that have created the opportunity for more care at home, including the growth in virtual care, remote monitoring, telehealth, social support, and home modifications, may enable more patients to receive some level of care at home.
Factors that could affect the adoptions of the growth of home care services are dependent on the following:
• Evaluating the services that can be delivered at home
• Economic viability for the healthcare facilities and physician groups
• Physician awareness, perceptions, and capabilities
• How patients feel about homecare
The COVID-19 pandemic has created a catalyst to fundamentally reimagine care at home to help improve the quality of care and patient experience while also creating potential value for payers, healthcare facilities and physician groups, home care providers, technology companies, and investors.
Patient care in their homes provides comfort for the patient and a reduced cost for Medicare; however, it needs to be appropriate and not be at the expense of preventable adverse health events. MLAP understands the risk intricacies in post-hospital discharge needs and the appropriateness of the discharge. Let us share our expertise with you to gain further insight into the standard of care in this process.
Assistance with Assisted Living
Tuesday, February 21st, 2023
Assisted Living Facilities (ALFs) began to pop up in the early 1980s. Since then, they have become a prominent provider of care for the elderly population. As this level of care has risen in popularity, so too have liability claims in this setting.
Levels of Care
Unlike nursing homes or skilled nursing and rehabilitation facilities, which provide medical care, residents appropriate for admission to ALFs do not require high-level medical monitoring or consistent medical care. ALFs provide care for seniors who require personal care assistance. This includes assistance with activities of daily living (ADLs) such as bathing, dressing, and eating. Seniors residing in assisted living facilities are also often provided help with meals, housekeeping, laundry, and medication assistance. One of the appealing aspects of ALFs is that residents can access as much or as little assistance as they need, allowing them to retain much of their independence and autonomy. Emphasis is frequently placed on providing ALF residents with activities to provide a more home-like environment and foster socialization. Most residents can enjoy the independence of individual apartments, often equipped with kitchens and handicap-accessible bathrooms. Many facilities also provide memory care services that are geared toward residents with Alzheimer’s disease or dementia.
Liability Claims in Assisted Living
The average cost of liability claims across all aging services settings has increased since 2018, with assisted living claim costs exceeding those of skilled nursing. Fall-related allegations were the most common in the assisted living setting. Fall-related injuries included fractures, head injuries, lacerations, muscle/ligament injuries, and death. Aside from falls, other frequent allegations in the assisted living setting were resident abuse, understaffing, failure to monitor or supervise, pressure injuries, delays in seeking treatment or failure to transfer, medication errors, elopements, and wrongful death. While pressure injury allegations are not prevalent in the assisted living setting, the severity of pressure injury claims has increased significantly. Elopement-related claims accounted for the smallest number of claims but were the most expensive. In an effort to curb litigation risks and enhance the quality of care and life of residents, risk management recommendations often include expectations management, clear and transparent communication with residents and families, and ensuring placement suitability.
Unlike nursing homes or skilled nursing and rehabilitation facilities, which are regulated by The Centers for Medicare and Medicaid Services (CMS), most ALFs are licensed and regulated by individual state health agencies. The team of legal nurse consultants at Med Law Advisory Partners is well-versed in the regulations specific to assisted living facilities. This knowledge is crucial when addressing allegations in these liability claims. Let us share our expertise with you to gain further insight into the standard of care in the assisted living setting. Our nurse consultants can make the difference in obtaining a favorable outcome in the defensibility of these cases.
All Long Term Care – or Risk of Liability – Is Not Equal
Friday, February 3rd, 2023
Recently, while coordinating the admission of a clinically appropriate patient to a long-term acute care hospital following treatment in an intensive care unit, a physician was reluctant to discharge the patient to long-term acute care. The reluctance came from believing that the patient would never achieve ventilator liberation. Unfortunately, this misconception is common. However, ventilator weaning is precisely what would occur in a long-term acute care hospital (LTACH) setting. In fact, the LTACH model of care specifically caters to the post-intensive care needs of critically ill, mechanically ventilated patients with complex needs and multiple serious diagnoses, necessitating collaborative, multi-disciplinary treatment, including hemodialysis, LVAD, and intense, aggressive specialized care and therapy, which cannot be provided in a short-term acute hospital setting.
Extended Intermediary Care
All long-term care is not the same. Although an LTACH is a form of long-term care, it is a medically complex transition from the acute care hospital intensive care or step-down unit to a longer-term, goal-focused, and outcome-directed plan of care for critically ill patients in need of extended recovery. LTACH care aims to provide continued treatment that cannot be offered in a skilled nursing facility or nursing home. Unlike those settings, an LTACH provides 24-hour physician support in addition to the auxiliary laboratory, radiology, telemetry, high acuity, and surgical care provided in a traditional acute care hospital, but on an extended basis. LTACH is the intermediary level of care provided before discharge home for further rehabilitation or a traditional long-term care setting.
The Importance of Interdisciplinary Care
Since the LTACH patient is often medically fragile and complicated, there are increased areas of liability involved in their care, as well. The highly collaborative nature of LTACH treatment means the interdisciplinary care team must work closely to ensure that goals of care are met timely, appropriately, and within the standard of care. While the goals consist of the traditional long-term care objectives of safety, nutrition, and skin integrity, the added complexities of critical illness correlate with an increased risk of liability when those goals remain unmet or are further complicated by ongoing issues. Thus, the collaboration of the interdisciplinary care team remains the core of LTACH care in meeting patient care needs through achieving maximum recovery potential, goal setting, and quality outcome measurement. In the immediate intensive care unit setting, outcomes are measured in shorter terms – minutes, hours, and days. The intensive care unit is a sprint. LTACH treatment, though, is the beginning of the marathon to recovery. Outcomes are measured over weeks and sometimes months, ultimately leading to longer-term recovery at skilled nursing facilities, nursing homes, and at home. The standard of care is the same as in the short-term hospital setting; however, the risk management challenges are more complex.
MLAP understands the risk intricacies involved in all aspects of long-term care, including long-term acute care hospital treatment. Let us share our expertise with you in gaining further insight into the standard of care involved in complex post-intensive care patient needs, ventilator liberation, complicated wound care treatment, and management of multiple critical diagnoses.
In a river of polluted medical data, let’s start a cleanup operation.
Monday, November 7th, 2022
We swim in a river of information.
Every day, we sort through data as we figure out what’s best for patients and the health care organizations we lead. It allows us to figure out the best treatments for folks while giving us an organization-wide perspective.
At least it should.
Too often, the data we’re swimming through is polluted. The gunk could come from disparate systems not lining up or poorly communicating information from one to the other. On the other hand, it might simply be outdated, so many dead fish floating alongside us in the murky water.
So let’s clean up that river. Let’s dig into that mucky, fetid swamp. Here are the main pollutants organizations face, along with a path forward.
Pollutant one: Poor data processing for patients
When it comes to treating patients, the central contradiction providers face is this: Data means everything, but the systems for collecting and accessing it vary wildly. Electronic health records have been haphazardly implemented worldwide and also bring associated security risks, while old-fashioned paper files are limited to their time and place.
Or as Kasaw Adane, Mucheye Gizachew and Semalegne Kendie wrote in Risk management and Healthcare Policy back in 2019:
“Poor medical data processing systems are the key reasons for medical errors. Employing standardized data management systems reduces errors and associated sufferings. Therefore, using electronic tools in the healthcare institution ensures safe and efficient data management. Therefore, it is important to establish appropriate medical data management systems for efficient health care delivery.”
Sounds simple enough, right? Make the transition and swim in the pure, clear water.
The authors even suggest that “effective use of EHR improves the patient’s safety, trust, and their satisfaction on the health care system appeared orienting patients towards a health-related information sources.”
Unfortunately, the security risks mentioned above continue. And electronic records adoption has lagged around the globe. Physicians don’t always believe in the platforms or have the time or interest to learn them. Moreover, a whole legal framework exists for understanding and grappling with these records.
Finally, even if you have an extant electronic health records system, it may not be sufficiently integrated into your organization. Fixing problems and setting goals depends on using that information correctly. And that leads us to our second pollutant.
Pollutant two: Feeding big data the right information
Electronic records serve individual patients. But if those records can be brought together with hundreds, thousands or millions of other patients’ records, you have a truly game-changing medical breakthrough.
Why? Think of it this way. Other patients’ experiences can inform the treatment of any individual. And other overall pictures can help institutions figure out what works and what doesn’t.
“Big data analytics has enabled doctors to access a holistic view of a patient’s health history,” writes Dmytro Spilka for Smart Data Collective. “Additionally, patients may find themselves more empowered with information and are taking charge of their personal health through big data insights.
“This trend has enabled doctors to design accurate intervention programs to treat diseases long before they can progress to more complex advanced stages that can be expensive and difficult to treat. Big data analytics is actively shifting healthcare delivery paradigms away from a reactive approach and more to a preventative approach.”
Sean Parker, writing for the same publication, notes that healthcare organizations can become more competitive by crunching numbers and communicating better.
The overall result? More profits.
But that doesn’t mean that you’re swimming through peaceful waters. Oh no. You will be faced with data entry and collection problems across the board. You will be faced with outdated computer systems and IT infrastructure resistant to the kind of innovations necessary.
“Inefficient data entry and collection practices are a significant source of waste among care providers and healthcare organizations,” Parker writes. “Advanced data collection technologies enable providers to automate many of these redundant practices. This will result in savings for healthcare organizations.”
Cleaning the river for everyone
Making sure that the data we all swim through works will take a collective effort.
That’s why a firm like Med Law Advisory Partners exists, to help you figure out your system pitfalls and how to clean your stream or river or ocean to near transparency.
As Alicia Davis, RN, LNCC, the founder and CEO of Med Law, puts it:
“We can stay ‘downstream’ in reactive mode, monitoring the increase in severity of patient harm events and repeatedly defending the same claims as we watch claim values continue to rise. Or, through innovation, problem-solving and creatively managing our resources, we might have the opportunity to improve ‘the way we’ve always done it’ – with the goal of driving down the cost of care delivery, building more efficient systems, increasing team member satisfaction, and, ultimately, having safer, healthier patients and communities.”
Together, we can make our processes and data work for us the right way. We can ensure that providers and caregivers have modern and efficient systems and that the information they collect helps the patients and our organizations thrive.
Our patients and providers deserve no less.