Archive for the ‘LTC’ Category
Universal Precautions vs. Standard Precautions
Thursday, February 18th, 2021
Most healthcare lawsuits involve a deviation from an established standard of care. To some extent, all medical centers and care facilities have policies in place to prevent the spread of infection. But are their guidelines up to date in light of recent public health issues? Is a provider’s infection control program making all reasonable efforts to guard against pandemics or contagious diseases that are either rare or unheard of? Are processes streamlined to ensure safety when a health professional is cut with “sharps” or splashed with body fluid?
In examining a case, legal teams search for evidence that a facility has – or has not – followed the most current health guidelines to protect staff, patients, and the community at large from infectious disease. Two similar terms pop up in legal research: Universal Precautions and Standard Precautions.
To understand both these terms, attorneys and paralegals must first consider the two main types of pathogen transmission: bloodborne and airborne.
Universal Precautions
In 1983, Centers for Disease Control (CDC) published the Guideline for Isolation Precautions in Hospitals. One section, “Blood and Body Fluid Precautions,” encouraged in-hospital healthcare workers to adhere to these precautions when a patient was known or suspected to be infected with a bloodborne pathogen like HIV or Hepatitis B.
The CDC followed up with Recommendations for Prevention of HIV Transmission in Health-Care Settings in August 1987. These 1987 recommendations encouraged the use of blood and body fluid precautions for all patients regardless of their infection status.
The extension of precautions to all patients was referred to as Universal Precautions. Under these guidelines, blood and body fluids of all patients were considered potentially infectious. Universal Precautions specified the use of gloves and face shields and avoiding exposure with needles and other instruments after use when the potential for contact with blood and bodily fluids was anticipated. The importance of frequent handwashing was at the core of these recommendations.
By 1987, a set of rules known as Body Substance Isolation (BSI) was added. It expanded the concept of personal protective equipment to include plastic aprons and covers for hair and shoes to keep all moist body substances off hair, skin, clothes, and mucous membranes. BSI went beyond simply discarding needles in puncture-resistant containers to placing them in puncture-proof containers. Hands were to be thoroughly washed before as well as after patient care and wearing gloves. Body Substance Isolation utilized hospital gowns, medical gloves, shoe covers, safety goggles, and surgical masks or N95 respirators. However, there was not a consistent interpretation or use in either BSI or universal precautions.
Standard Precautions
Times have changed since Universal Precautions were first set in place. The 21st century has seen devastating illness from Ebola virus, avian flu, West Nile virus, SARS, Zika virus and biological warfare as well as the pandemic flu from previous generations. Gloves alone do not completely protect a health professional or patient. Even diseases usually transmitted by contact can be aerosolized by saliva and respiratory secretions. Irrigating a wound can risk a splash back of fluid. Respirator masks can be contaminated. Today, public health officials must prepare against contact and airborne transmission as well as bloodborne risks.
In 1996, the Centers for Disease Control and Prevention established the term Standard Precautions. This broadened the focus on prevention, applying the principles to all patients regardless of diagnosis or presumed infection status. These guidelines consider the risk of transmission of illness from both recognized and unrecognized sources.
In the very simplest terms, Standard Precautions involve washing hands before and after patient contact, whether or not gloves are worn. They involve wearing clean gloves when touching blood, body fluids, and contaminated items, as well as a clean, non-sterile gown and a mask, eye protection or face shield in the likely event of splashes or sprays. Soiled equipment and linen are carefully handled to prevent injuries from used equipment.
These measures are the minimum infection prevention practice applying to all patient care, regardless of the healthcare setting or whether a patient is known or suspected to carry disease.
Transmission-Based Precautions
Transmission-Based Precautions are the second tier of basic infection control and are to be used in addition to Standard Precautions for patients who may be infected or colonized with certain infections, including the virus that causes COVID-19, for which additional precautions are needed to prevent infection transmission. Those include Contact Precautions, Droplet Precautions, and Airborne Precautions. Each have specific guidelines and applications which must be addressed in policy and followed by staff to avoid legal ramifications.
Universal Precautions vs. Standard Precautions
In summary, universal precautions involve precautions taken with all patients, regardless of suspicion of infection, to prevent the spread of bloodborne pathogens. In an inevitable evolution, standard precautions, in contrast, are steps taken to encompass fighting the spread of airborne pathogens in situations where providers come into contact with any form of body fluid. Transmission-Based precautions are more specific and used in addition to standard precautions when certain infections are present. The type of precaution applied in a facility is essential to most medical malpractice and healthcare-related claims. Understanding the difference is key both for healthcare providers and legal teams.
The presence or absence of a “safety culture” (also known as a safety climate) promoting appropriate infection precautions is a key component in any medical malpractice case. Med Law’s team of nurse consultants can help pinpoint whether a provider has been in compliance and can be a strong partner in pursuing or defending a medical malpractice suit. We’d love to chat with you – contact us today to schedule a conversation.
Med Law Advisory Partner’s team of medical-legal consultants can help you pinpoint whether a provider has been in compliance and be your best foot forward in pursuing or defending a medical malpractice suit. We’d love to chat with you – contact us today to schedule a conversation.
 Founded by Alicia Davis, RN, LNCC, Med Law Advisory Partners (formerly ALN Consulting) provides resources and expertise in the areas of health care litigation and health systems improvement. Med Law Advisory Partners’ team has had the privilege of working with national and regional healthcare systems, legal firms, insurers, and senior-living operators for nearly 20 years, providing medical-legal case investigation.
Founded by Alicia Davis, RN, LNCC, Med Law Advisory Partners (formerly ALN Consulting) provides resources and expertise in the areas of health care litigation and health systems improvement. Med Law Advisory Partners’ team has had the privilege of working with national and regional healthcare systems, legal firms, insurers, and senior-living operators for nearly 20 years, providing medical-legal case investigation.
Originally published July 29, 2016. Post last reviewed and updated Feb. 18, 2021.
What Plaintiff’s Attorneys Need to Know About DOJ and OIG Investigations of LTC Facilities
Thursday, April 26th, 2018
In a recent post, we wrote about how government funds available for The Health Care Fraud and Abuse Control Account have more than doubled since 2009— going from $465 million to more than $963 million. At the same time, funds dedicated to Department of Justice (DOJ) investigations have more than tripled from $198 million to $681 million. Long-Term Care (LTC) facilities and providers defend against DOJ and Office of Inspector General (OIG) investigations of Medicare/Medicaid fraud, allegations of “worthless care,” allegations related to the False Claims Act, and other similar investigations still in litigation.
Why should Plaintiff’s Attorneys care about this trend in litigation?
Enacted during the Civil War and amended several times, the False Claims Act (FCA), 31 U.S.C. §§ 3729 – 3733 provides that any person who presents a false or fraudulent claim for payment or approval to an officer or employee of the United States government or otherwise engages in certain enumerated fraudulent activities is liable to the government for a civil penalty of not less than $5,000 and not more than $10,000, plus three times the amount of damages which the Government sustains because of the act of that person. The 1986 amendment to the FCA allows private persons to file suit for violations of the FCA on behalf of the government. A suit filed by an individual on behalf of the government is known as a “qui tam” action and the person bringing the action is referred to as a “relator.” If the government intervenes in the qui tam action, the relator is entitled to receive between 15 and 25 percent of the amount recovered by the government. If the government declines to intervene in the action, the relator’s share increases to between 25 to 30 percent.
Early in 2018, the Department of Justice released a memo to give DOJ litigators a “general framework” of factors to consider when deciding whether or not to dismiss False Claims Act cases brought by qui tam relators on behalf of the government due to recent “record increases” in qui tam actions. For this important reason alone, Plaintiff’s Attorneys representing qui tam relators should have solid evidence of fraudulent claims before investing resources in such cases.
ALN Consulting nurses are experienced in such litigation and can provide analysis integral to successfully trying cases related to the False Claims Act. When reviewing allegations of worthless care, ALN Consulting looks at the overall care provided rather than analyzing specific events or breaches from standard care or level of harm — taking a much broader approach than those of typical litigation. In cases where a relator was unable to prove false or fraudulent claims, a sharp and detail oriented legal nurse consultant could have made the difference in the evidence presented.
We’ve done the research, so you don’t have to! ALN Consulting will continue to stay on top of these and other developments.
Have questions about a case? Setup a consultation with our experts.
How to Defend Long-Term Care Facilities Against DOJ and OIG Investigations
Thursday, September 7th, 2017
Since 2009, government funds available for The Health Care Fraud and Abuse Control Account have more than doubled — going from $465 million to more than $963 million. Funds dedicated for Department of Justice (DOJ) investigations have more than tripled from $198 million to $681 million. That said, Long-Term Care (LTC) facilities and providers must be equipped to defend against DOJ and Office of Inspector General (OIG) investigations of Medicare/Medicaid fraud, allegations of “worthless care,” allegations related to the False Claims Act, and other similar investigations still in litigation. ALN Consulting has extensive experience in delivering results for firms facing these investigations.
During an investigation, LTC facilities and providers need seasoned nurse experts, who can review care and uncover demonstrative evidence that shows whether a patient’s care was optimal. ALN Consulting nurse reviewers can help your team defend against DOJ and OIG investigations of fraud, false claims and worthless care allegations.
In one case, the United States claimed $18, 710, 000 in damages for Medicare and Medicaid failure. ALN Consulting nurses stepped in to examine the care 28 residents in 5 facilities to determine evidence of excellent care and refute allegations. During this review, ALN Consulting nurses probed Pre-Admission Evaluations (PAE) and Pre-Admission Screening and Resident Review (PASRR) in multiple facilities. The results revealed only 36 percent of the cases were assessed damages by the government after ALN nurse reviewers created demonstrative evidence of care. By implementing the ALN Consulting team, it reduced the damages to 20 of the PAE’s and 6 of the PASRR cases.
“In recent years, in part through the Affordable Care Act, the Department of Justice and the Centers for Medicare and Medicaid Services has attempted to refocus efforts on identifying and stopping Medicare fraud,” Gregory Stevens, a professor at the University of Southern California who specializes in health care reform and policy, told the Louisiana Record. “And each year, tens, if not hundreds, of individual physicians are singled out and prosecuted.”
“It is often difficult to clearly establish that what was billed to Medicare inaccurately was done so intentionally,” Stevens said. “Billing is complex and even well-meaning providers can have a pattern of billing Medicare that is not accurate.”
When reviewing allegations of worthless care, ALN Consulting looks at the overall care provided rather than analyzing specific events or breaches from standard care or level of harm — taking a much broader approach than those of typical litigation.
In one particular investigation, the ALN Consulting reviewers looked at medical records to determine whether worthless care was provided to a resident of a LTC facility. In this case, the DOJ/OIG made allegations of worthless care related to a resident’s poor hygiene, medication errors and poor nutrition. After reviewing records — while they did show some evidence of failures to care plans, omissions to medication administration and evidence of bed baths rather than showers — the overall record proved consistent care was provided.
Special News Bulletin Pt 1: 2017 Interpretive Guidelines for LTC Surveyors
Monday, July 31st, 2017
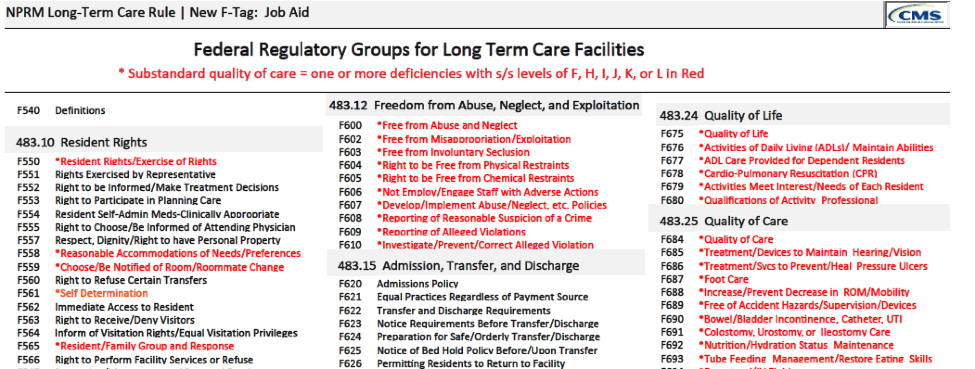
In September 2016, the Centers for Medicare and Medicaid Services (CMS) released the revised Requirements for Participation and Reform of Requirements for the Long-Term Care Facilities rule. The new regulations reflected advances in the theory and practice of long-term care service delivery and safety, and implemented sections of the Affordable Care Act. The overarching themes of the Final Rule were person-centered care and quality; utilizing a facility assessment competency-based approach; care planning from a person centered perspective; alignment with HHS initiatives; comprehensive review and modernization; and implementation of legislation. The rules were re-organized and updated, making them consistent with current health and safety knowledge.
In light of the implementation of these new regulations surveyors, facilities, practitioners, as well as those in the legal field involved in long-term care and skilled nursing care litigation have been eagerly awaiting the new Interpretive Guidelines for details. These guidelines are effective November 28, 2017, and CMS released the revised version of Appendix PP (interpretive guidelines for surveyors) in advance of the implementation date for Phase 2 of the CMS revisions. Research of these changes can be challenging and tedious, but ALN Consulting stays on top of all of the regulation changes and interpretive guidelines so that each review uses the most up-to-date information available. In Part 1 of this ALN Special News Bulletin, we will give you an overview of the new Interpretive Guidelines and revised F-Tags. In Part 2, we will delve deeper into the particulars of the changes and implementation.
Revised Interpretive Guidance – Appendix PP
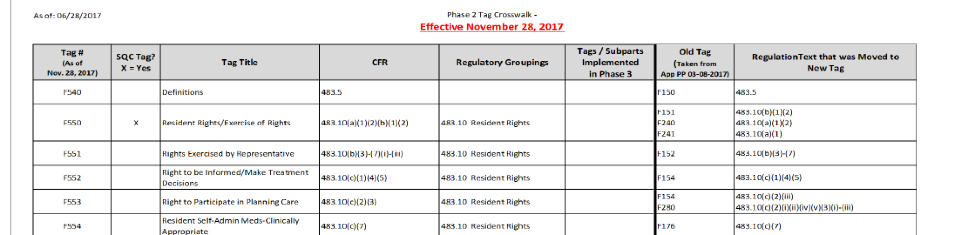
The new changes are effective November 28, 2017, and until then providers and surveyors will continue to use the revised version of Appendix PP released March 8, 2017. The CMS Medicare Learning Network created an “F-Tag Crosswalk,” a tool for users to identify new tag numbers, cross referenced with old tags, and the regulation text that was moved to the new tag:
According to CMS, many standards have remained unchanged since the early 1990’s. CMS updated the existing guidelines where necessary, and added a section in some areas to the Interpretive Guidelines titled, “Key Elements of Noncompliance” intended to guide surveyors and LTC facilities about the key behaviors and practices identified in the regulation.
Quality of Care F-Tags
A revised list of the F-Tags under each regulatory group is now available for use. The regulations were re-structured: some tags combined, and some tags split into multiple subparts.
An example of an F-Tag which changed is F600 – Abuse and Neglect, which combined into a single tag. Additional guidance clarified what constitutes abuse and neglect; assessing consent; involuntary seclusion; physical and chemical restraints; policies to prohibit abuse and neglect; and reporting requirements.
The new F684 – Quality of Care Tag was formerly F309 – Hospice, palliative care, and other care issues. It now contains guidance on dialysis, respiratory care, fecal incontinence, position change alarms, and bed rails.
New guidance for Infection Control includes discussion of an “Antibiotic Stewardship Program,” to encourage minimum antibiotic use protocols and a system for monitoring antibiotic use based on CDC guidance.
Enforcement of New Regulations
CMS released a statement confirming they “heard concerns regarding the scope and timing of the new requirements for Phase 2. We believe that these standards (for example, development of an antibiotic stewardship program to combat multi-drug resistant organisms) represent important national health and safety standards. However, to address these concerns, CMS will provide a one-year restriction of enforcement remedies for specific Phase 2 requirements. Specifically, we will not utilize civil money penalties, denial of payment, and/or termination. Should a facility be found to be out of compliance with these new requirements beginning in November of 2017, CMS would use this year-long period to educate facilities…by requiring a directed plan of correction or additional directed in-service training. Enforcement of other existing standards (including Phase 1 requirements) would follow the standard process.”
CMS has not released the listing of specific Phase 2 requirements associated with enforcement delays. However, this will present a unique challenge to litigation focused on this period for both Plaintiff and Defense alike. The requirements will be implemented, but not all enforced equally. Review of records with allegations pertaining directly to the regulation changes should be handled with a keen eye toward the changes implemented by the facility, and also toward specific correction plans if applicable.
We’ve done the research, so you don’t have to! ALN Consulting will continue to stay on top of these and other developments. Contact ALN Consulting if you have questions about a case and would like an initial consultation.
Sources
Interpretive Guidelines, CMS Revision to SOM Appendix PP, effective 11/28/17
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/GuidanceforLawsAndRegulations/Downloads/Advance-Appendix-PP-Including-Phase-2-.pdf
Interpretive Guidelines, CMS Revision to SOM Appendix PP, effective 03/08/17
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/GuidanceforLawsAndRegulations/Downloads/Appendix-PP-03-08-2017.pdf
CMS Revised F-tags,
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/GuidanceforLawsAndRegulations/Downloads/List-of-Revised-FTags.pdf
Final Rule, Federal Register, October 4, 2016.
https://www.gpo.gov/fdsys/pkg/FR-2016-10-04/pdf/2016-23503.pdf
MLN Revised Interpretive Guidance for Nursing Homes and New Survey Process
https://www.cms.gov/Outreach-and-Education/Outreach/NPC/Downloads/2017-07-25-NH-Presentation.pdf
Medical Malpractice and Long-Term Care: Plaintiffs
Monday, July 24th, 2017
This is the second installment of our two-part series looking at medical malpractice cases in long-term care, from the perspectives of both the defense and the plaintiff. Click here to read Medical Malpractice and Long Term Care: Defense.
Each season brings a new chapter in the legal battle over caps on medical malpractice claims. Recently, the Florida Supreme Court ruled that capping damages on pain and suffering in these cases is unconstitutional. The new ruling overturns a controversial law that the state legislature and governor affected back in 2003. Even more recently, a Wisconsin appellate court declared its own state’s malpractice claim cap unconstitutional. This means that the State of Wisconsin will no longer limit noneconomic damages in medical malpractice cases to $750,000.
But where some limits on plaintiff damages are struck down, other roadblocks materialize. The State of Kentucky now requires a panel of medical providers to evaluate claims filed against healthcare providers, including long-term care facilities. Patients and their families who want to seek legal damages from a care facility must now go before a panel before they can go to court. The evaluator’s opinions are eligible to be used as evidence in subsequent litigation. This and other legislation could not only reduce monetary compensation but also delay plaintiffs’ access to the circuit court for months.
On the federal level, a bill passed in the U.S. House of Representatives, the Protecting Access to Care Act of 2017 (H.R. 1215), would limit both damages and attorney fees as well as modify statutes of limitations in medical malpractice claims. Non-economic damages in medical malpractice lawsuits would be limited to $250,000. Moreover, juries would not be made aware of this cap on damages. If enacted, H.R. 1215 would apply to litigation where healthcare coverage was provided or subsidized by the federal government, including through subsidies or tax benefits.
Arbitration Agreements
New legislation could have a tremendous impact on anyone whose loved one has received improper care or suffered an adverse medical event in a nursing home, assisted living center, or in other long-term care. Last fall, the Final Rule put forth by the Center for Medicare and Medicaid Services (CMS) stated that LTC facilities could not require clients to sign pre-dispute arbitration agreements, which aim to prevent residents and their families from suing over care issues. At this time, CMS is reconsidering this rule after the American Health Care Association challenged the rule in federal court and was granted a preliminary injunction in district court. CMS has published a new rule, the revisions of which include the removal of the prohibition on LTC facilities requiring residents sign an arbitration agreement as a condition of admission to a facility.
An Uncertain Future
Recent caps on medical malpractice damages suggests that claimants seeking relief from a long-term care provider may find the odds against them. It is unclear how long legislative battles may drag on, or what other U.S. states may follow suit with medical malpractice bills. This makes it all the more challenging – and all the more important – for plaintiff attorneys to fight vigorously for their clients’ interests.
To prevail against a long-term healthcare provider, the plaintiff must first establish that the LTC facility has breached the industry standard of care. The defense will counter with any evidence that the facility was in compliance with the standards of care or, in the case of any breach in the care standard, that they were not responsible for the adverse outcome that prompted the lawsuit.
An Expert to Challenge Their Experts
The plaintiff will counter by challenging the defense team’s expert testimony. As with other litigation, medical malpractice and long-term care cases often pit one expert against the other. This means calling the most relevant expert witnesses available to support the case. Nursing expertise is ideal in cases of LTC-related medical malpractice.
The next challenge is to justify the amount of damages the claimant is seeking. This means meticulously documenting not only the physical changes now, but problems he or she will likely have in the future. The less obvious the effects on a patient’s health, mobility and life, the greater the burden on the plaintiff’s legal team to prove that the damages sought are reasonable. Quantifying the pain and suffering of a living facility resident is not easy, to say nothing of a deceased patient who cannot testify on his or her behalf.
The Best Investment for Your Time
Attorneys lack the time – and paralegals and jurors lack the acumen – to painstakingly review and evaluate lengthy medical records. This calls for a skilled medical-legal professional to bridge the gap. Legal nurse consultants distill the facts to their essence while providing constructed evaluations, analyses, and case histories. They provide precise, comprehensive information that attorneys can use and jurors can understand.
While medical malpractice caps and other changes affecting long-term care patients are evolving, a legal nurse consultant can be the best weapon in your arsenal. Contact us to learn more how you can put the ALN Consulting team to work for you.
Sources
“Wisconsin’s cap on medical malpractice awards unconstitutional, courts rules,” Milwaukee Journal-Sentinel, July 5, 2017
http://www.jsonline.com/story/news/investigations/2017/07/05/wisconsins-cap-medical-malpractice-awards-unconstitutional-courts-rules/451418001/
“Malpractice damage caps struck down by Florida Supreme Court,” Orlando Sentinel, June 8, 2017.
http://www.orlandosentinel.com/news/politics/political-pulse/os-malpractice-damages-20170608-story.html
“Lawsuit challenges new law aimed at limiting medical malpractice lawsuits,” Lexington Herald-Leader, July 6, 2017
http://www.kentucky.com/news/politics-government/article159985419.html
“Florida justices eye constitutionality of malpractice caps,” Palm Beach Post, June 9, 2016
http://www.palmbeachpost.com/news/state–regional-govt–politics/florida-justices-eye-constitutionality-malpractice-caps/TomuNdKwsg6wTE2mjPK5gN/
“House passes medical malpractice bill,” Washington Examiner, June 28, 2017
http://www.washingtonexaminer.com/house-passes-medical-malpractice-bill/article/2627374
“CMS lifts ban on nursing home arbitration agreement,” Modern Healthcare, June 5, 2017
http://www.modernhealthcare.com/article/20170605/NEWS/170609949/cms-lifts-ban-on-nursing-home-arbitration-agreement
Medical Malpractice and Long Term Care: Defense
Wednesday, June 21st, 2017
We’re kicking off a two-part series looking at medical malpractice cases in long-term care, from the perspectives of both the defense and the plaintiff.
Part 1: The Defense of Long-Term Care Facilities
When a defense team defends a long-term care facility against medical malpractice, one of the first questions to ask is: “Did this facility and its medical professionals adhere to an established standard of care?” New requirements in the Final Rule put forth by the Center for Medicare and Medicaid Services (CMS) complicate this question more than ever.
Last fall, long-term care (LTC) facilities faced the first major overhaul of federal participation requirements since 1991. The Final Rule produced new specifications on features of a facility’s building and staffing ratios. Long-term care centers must now develop compliance and ethics programs as well as Quality Assurance and Performance Improvement (QAPI) initiatives. For a nursing home or assisted living center, this now means assessing the full spectrum of patient care from staff members’ skill sets and training to the right environment, equipment, health information technology, and other resources.
The Final Rule also stated Medicare and Medicaid certified long-term care facilities must not enter into an agreement for binding arbitration with a resident or their representative until after a dispute arose between parties. An industry group challenged CMS’s legal authority and won a preliminary injunction in federal court, and the Trump administration ultimately dropped the matter and chose not to appeal to the U.S. Supreme Court, essentially ending the ban on pre-dispute arbitration agreement use in long-term care.
As standards change, liability remains the same.
The next phase of Final Rule regulations takes effect this November, with the final changes to come in 2018. All of this new regulated compliance may mean more – and different – ways that care providers can trip up and land in legal hot water.
But in any case, law firms will continue to represent nursing homes and assisted living facilities in legal disputes over care, including medical malpractice allegations. Even with federal efforts to put a cap on medical malpractice awards, these cases can wreak havoc on care providers and their insurers even in the best of circumstances.
With such high stakes, LTC facilities must be more than CMS-compliant. They must be prepared to defend themselves in the face of medical malpractice litigation with the best expert witnesses for their case, as well as establish medical facts in a way that jurors with no medical background can comprehend. These are both tasks which legal nurse consultants (LNC’s) are in a unique position to fulfill.
An expert who recommends other experts.
A legal nurse consultant will cull all medical, employment, invoices, and deposition testimony. He or she will identify missing pieces, such as absent records, for the defense attorney to request. At that point, the LNC can recommend the most suitable medical professionals to explain and defend against the plaintiff’s allegations.
The importance of making facts understandable to lay jurors should not be underestimated. In a medical malpractice case overturned last month by the Missouri Supreme Court, the initial judge threw out the patient’s informed consent agreement because it “could only confuse the jury in its determination of the facts.”
In most malpractice cases, medical jargon is too intricate for lay jurors to fully grasp. The LNC behind the scenes, and experts on the witness stand whom he or she identifies, will walk the jury through the details to understand why a lawsuit was filed, and why the defendant is not liable.
Causation is key
Once a legal team has fully addressed the “standard of care” question, it must address what caused the adverse outcome. Should a deviation from the care standard be found, did it result in the issue for which the plaintiff seeks damages?
In yet another recent case, an Ohio appeals court ruled in favor of a skilled nursing facility in a medical malpractice case, vacating the $1 million in damages and attorney fees from the original trial two years ago. A deceased resident’s estate administrator attributed her death to staff negligence, as well as pressure wounds and “fatal” injuries that were not reported to her family or doctor.
The LTC center filed a motion for a new trial, as well as a reduction in damages, which was denied the following year. But the defense appealed – and the appellate court ruled in their favor, citing insufficient evidence that they intentionally acted, or failed to act, knowing that substantial harm would likely result. Further, the judge found no evidence of ill-will or a spirit of revenge when caring for the woman.
This is the type of long-term care malpractice case where a legal nurse consultant can make a real difference in the outcome. In a case like this, the LNC would review the resident’s medication history and progress notes of physicians and nurses. Establishing causation takes more than checking vital signs and scanning a medical record. It is important not only to research a facility resident’s prescribed diet (which is now a requirement in CMS compliance), but whether or not the resident has adhered to that regimen and eaten the food the long-term care facility has provided. This puts the defendant in the best possible position to challenge financially devastating litigation.
As with the two cases in Missouri and Ohio, a serious allegation – and even losing one legal battle – does not mean that a defense team can’t eventually prevail. Your best weapon can be a legal consultant with a nursing background – and a full command of the details and nuances of a seemingly straightforward medical event. With a strong knowledge of regulatory changes in the long-term care landscape, a legal nurse consultant can help a legal team build a strong defense for the client.
Sign up for our email updates so you don’t miss the second part in our series on Malpractice in Long-Term Care outlining how a legal nurse consultant can improve a the Plaintiff’s case in long-term care litigation. ALN Consulting will continue to stay on top of these and other developments. Contact ALN Consulting if you have questions about a case and would like an initial consultation.
Sources
Final Rule, Federal Register, October 4, 2016. https://www.gpo.gov/fdsys/pkg/FR-2016-10-04/pdf/2016-23503.pdf
“Medicare Backtracks on Long Term Care Arbitration Rule,” Bloomberg BNA, June 6, 2017. https://www.bna.com/medicare-backtracks-longterm-b73014451967/
“Federal Efforts to Cap Medical Malpractice Awards Stall,” June 8, 2017. The Legal Examiner. http://virginiabeach.legalexaminer.com/medical-malpractice/federal-efforts-to-cap-medical-malpractice-awards-stall/
“Missouri Supreme Court Gives New Life to Medical Malpractice Case,” Legal Newsline, May 31, 2017. http://legalnewsline.com/stories/511120653-mo-supreme-court-gives-new-life-to-medical-malpractice-case
“Court Grants Nursing Home a Win in Appeal of $1 Million Medical Negligence Suit,” McKnight’s Long Term Care News, May 1, 2017. http://www.mcknights.com/news/court-grants-nursing-home-a-win-in-appeal-of-1-million-medical-negligence-suit/article/653732/
Geriatric Sexual Assault: An Elder Abuse Phenomenon
Thursday, March 16th, 2017
There is a nearly invisible injustice occurring in the United States today. It’s a subject no one ever wants to think about: rape. But, more than that, it’s happening to someone we never thought it would: our parent. Namely, our mothers and grandmothers. Even more, it’s happening in a place we never thought it would: their nursing home. Yes, we have heard the nursing home horror stories of inadequate care, but this is more evil and horrifying than even those news headlines.
Recently, CNN Investigations published an exposé that brought up an important yet disturbing fact: most elderly rape cases in assisted living facilities and hospitals are never reported to authorities. Many aren’t even investigated. They are simply forgotten and again (like we’ve seen in other claims of rape), victims are blamed. There are many reasons given for why a facility leaves the case unsolved: She has dementia. It must have been a delusion, a hallucination. She doesn’t even remember what exactly happened. He doesn’t have a record of abuse…
The unfortunate truth, though, is that many of these perpetrators who work in these facilities have worked there for years and will continue to work there for many more years because there is no appropriate method of response. One perpetrator lied to a nursing home during his hiring process, and then later raped an elderly woman. He did not disclose the previous allegations of sexual assault against him at other facilities, and there were a number. Why are these nursing homes and hospitals not fully vetting their employees? Why are reports of abuse going undocumented? Why is the most evil of acts against the most vulnerable going unpunished? Why aren’t our elders protected in the places they live, the places they call home, by the people who are meant to care for them at the most intimate level?
There are recent reports on this horrific phenomenon that might help us get closer to the answers. Dr. XinQui Dong, MPH writes, “evidence suggests that one in 10 older adults experiences some form of elder abuse, but only one in 25 cases is reported to social services agencies” (Dong, 2012). Elder abuse includes many different kinds of mistreatment, and this is not just referring to sexual assault. But, the silence around reporting is a damage-inflicting status quo that needs correction.
The American Academy of Nursing on Policy said in 2015 that “elder mistreatment is a major national health concern.” This is especially important because it can be “contagious” in families and in certain environments. This is also because the elderly population is growing in size every day and baby boomers are slowly transitioning into being the largest elderly population our country has ever seen. This could lead to overcrowding of assisted living facilities and a lack of experienced medical and care professionals in those environments as well as lack of care at home, which could make elderly abuse an even bigger problem.
Even though nurses and other health care professionals would be perfectly-positioned people to keep watch over the elderly and report any sign of neglect or abuse, “they are…among the least likely to do so” (Schmeidel, Daly, Rosenbaum, Schmuch, & Jogerst, 2012). The Elder Justice Act of 2010, a part of the Patient Protection and Affordable Care Act, has brought attention to this issue, but Congress has not approved any of the funding the act requires.
How does elder mistreatment affect the elderly? The American Academy of Nursing on Policy says, “For the elder, the experience of mistreatment itself, in any of its forms, often also results in behavioral health symptoms including depression, risk of suicide, anxiety, cognitive dysfunction and sleep difficulty; self-treatment with drugs and alcohol; injuries and morbidities resulting in higher use of emergency department, hospital and nursing home services, and greater mortality (Dong, 2014).”
What is being done to combat this growing problem? An Elder Justice Roadmap (Connolly et al., 2014) was created in 2014 with assistance from the Department of Justice and the Department of Health and Human Services. This “Roadmap” is a guide to “strategic policy, practice, education and research initiatives that” advance the goals of the Elder Justice Act. The American Academy of Nursing on Policy draws from this Elder Justice Roadmap that the top priorities for moving forward are “prevention, recognition, and treatment,” as well as “education,” “training,” and “research.”
How do I report this?
National reports of abuse & neglect in nursing facilities made to the Long-Term Care Ombudsman went down by the thousands from 2006 to 2013. Sexual abuse reports started to go down in number from 2011 to 2013, but this does not mean that there were less sexual assaults to the elderly. Social scientists believe the current number of yearly reports are “only the tip of the iceberg” (Brosens, De Dondera, De Witte, Dierckx, Verte, 2014).
Every state has different rules and laws governing the requirements of who must report elder abuse, but most states at least require that medical professionals in closest contact with the elder, namely home health aides and physicians, are mandated “to report any suspected abuse or neglect” (Haimowitz, Stefanacci, 2013). These “mandated reporters” must report any negligence that is intentional or unintentional for the protection of vulnerable senior citizens. In several states, “‘any person’ is required to report a suspicion of mistreatment” (Haimowitz, Stefanacci, 2013). This includes physical abuse, emotional abuse, sexual abuse, exploitation (of funds or assets), neglect, or abandonment.
Every state has an appropriate number of a department to call if you suspect elder abuse. You will need to provide the senior’s name, address, contact info, and details of what causes you concern. Be prepared for more questions about the elder’s medical history, family environment, and any signs of abuse. You may also be required to report to the facility you work in if you work for the elder in that capacity. You should report to the facility in any case. You may or may not be able to report anonymously; this also depends on your state. Always be on guard and watching, and always report suspicious activity around the care of an aging adult.
From LeAnne Smith, veteran R.N. and ALN Legal Nurse Consultant:
“In the last few years, I have evaluated potential cases which involved allegations of rape or sexual assault. In one case, a 53 year-old female nursing home resident, who was described as cognitively intact and had no history of psychiatric diagnoses, reported an attempted rape. The resident was assessed with no injuries identified, and the MD, family, and police were notified. The resident was transferred to a psychiatric facility for evaluation of delusions and returned to the facility the same day. The state was not notified and there was no investigation of the events on any level. It was simply forgotten.
In another case, an 80-year old female resident had reported inappropriate comments and touching by a male staff member. This was reported to a facility LPN, who told the resident to complete a “care concern report”. The LPN did not report the events to anyone, and the resident was not assessed for injuries. Two years after these events, the resident reported the events to Adult Protective Services (APS). APS investigated the report, and allegations were substantiated. The alleged perpetrator was fired, and the LPN who failed to investigate and report the events was disciplined for failing to comply with mandatory reporting of alleged abuse. There were other cases which were also handled in a similar manner.
My experience with cases involving rape or sexual assault allegations mirrored the findings in the CNN Investigation. It appears that allegations involving sexual assault or rape are not adequately reported or investigated, leaving the elder population at risk. Additionally, it appears the medical professions serving the elderly are not adequately trained in the appropriate process for reporting and investigating these types of allegations.”
What does the future hold?
The American Academy of Nursing on Policy (AANP) recommends the “expansion of Medicare/Medicaid reimbursement to better cover screening and basic first level mental health services by primary care provider staff.” This will detect mental health issues, substance abuse or misuse, and mistreatment to the elder.
The AANP also recommends that there be inter-professional training to combat and prevent ageist mistreatment, “mandatory continuing education for nurses on elder abuse,” prioritizing of a “research and program evaluation agenda,” disseminating of training materials, and intervening from Adult Protective Services. The AANP believes that the “effectiveness of preventive, early recognition, surveillance, intervention (including legal) and rehabilitative programs… including those with cognitive impairment” can work to end this sad epidemic.
CNN investigations report that this silent phenomenon of elder sexual assault is widespread and some medical and care facilities are “willfully” ignoring its existence. Strides to unveil what’s hiding in the dark, literally and figuratively, are being made, but please read more in our source list to learn how you can be an agent of change for the elderly. Medical professionals have an obligation to watch over, protect, and seek justice for our aging and ailing patients.
Sources:
“Sick, Dying and Raped in America’s Nursing Homes.” CNN. Cable News Network, n.d. Web. 08 Mar. 2017.
http://www.cnn.com/interactive/2017/02/health/nursing-home-sex-abuse-investigation/?iid=ob_homepage_deskrecommended_pool
Expert Panel on Aging, and Psychiatric, Mental Health & Substance Abuse Expert Panel. “Elder Justice: Preventing and Intervening in Elder Mistreatment.” Nursing Outlook 63.5 (2015): 610-13. Web.
Bloemen, Elizabeth M., Tony Rosen, Sunday Clark, Denis Nash, and Thelma J. Mielenz. “Trends in Reporting of Abuse and Neglect to Long Term Care Ombudsmen: Data from the National Ombudsman Reporting System from 2006 to 2013.” Geriatric Nursing 36.4 (2015): 281-83. Web.
Donder, Liesbeth De, Nico De Witte, Dorien Brosens, Eva Dierckx, and Dominique Verte. “Learning to Detect and Prevent Elder Abuse: The Need for a Valid Risk Assessment Instrument.” Procedia – Social and Behavioral Sciences 191 (2015): 1483-488. Web.
Dong, Xinqi. “Advancing the Field of Elder Abuse: Future Directions and Policy Implications.” Journal of the American Geriatrics Society (2012): n. pag. Web.
Stefanacci, Richard G., and Daniel Haimowitz. “What We Need to Report and to Whom.” Geriatric Nursing 34.1 (2013): 68-71. Web.
When Medicare Demands a Refund
Tuesday, January 17th, 2017
The Department of Health and Human Services, Office of Inspector General has been conducting massive fraud sweeps of its contractors and programs. With an eye to reducing waste and mismanagement, the HHS and OIG are now going after multi-site healthcare organizations like never before with a complete revamp of rules unseen in 15 years. And they’re not stopping on obvious quality of care abuses. These departments are auditing for past Medicare invoicing – and demanding refunds for services they have identified as over-billing. According to experts, small and mid-sized providers should be particularly alert to Medicare Secondary Payer Compliance since their billing systems are frequently not as advanced as hospital systems or large medical groups.
On November 30, 2017, the OIG posted its Semiannual Report to Congress, which is a summary of the OIG’s activities from April 1, 2017, to September 30, 2017. The Inspector General, Daniel Levinson, reported during FY 2017 the total figure of expected recoveries rose to $4.13 billion, and included criminal action against 881 individuals or entities that engaged in crimes against HHS programs, the exclusion of 3,244 individuals and entities from Federal healthcare programs, and civil actions against 826 individuals or entities.
As part of the OIG’s overall concerns about questionable prescribing of Medicare Part D, OIG and law enforcement conducted the largest National Health Care Fraud Takedown in history and charged 120 health care professional defendants for their roles in prescribing and distributing opioids. The government also charged than 400 defendants in 41 Federal districts with participating in fraud schemes involving about $1.3 billion in false billings to Medicare and Medicaid.
Defending Yourself Against Medicare Fraud Claims
But can an “overbilling” refund be challenged? Defending oneself against quality of care investigations is only part of the puzzle. Today, billing issues are quality of care issues. And comprehensive quality of care issues is how ALN has served clients for many years.
ALN Consulting takes a proactive approach to new governmental guidelines and looming audit possibilities. With HHS’s new guidelines in full force, we can review your current records and educate your staff about potential red flags in light of new HHS compliance. LNCs can determine what issues are avoidable and which are not. We offer the best possible preparation for an audit that could happen at any time.
But if the OIG contacts your office before your audit preparation is in place, ALN is ready to help you step by step. First, our legal nurse consultants will investigate the degree of accuracy of the governmental assessment. From there, we will work with you to develop a strategy and assemble appropriate clinical documentation to defend and manage against that claim. Our experienced consultants create case studies which support the beneficial services your staff has rendered and justify the so-called “overbilling” and “worthless service” claims that were flagged by the HHS.
Like many other industries, the healthcare and insurance communities must prepare themselves for audits of financial compliance as well as industry-specific issues. Mitigating a hefty government penalty is only part of the investment you make with your legal consultant. ALN can be your best defense against government bureaucracy…and groom you for the new normal in healthcare compliance.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.
Want to contact our experts? We would enjoy the chance to speak with you.
Kennedy Terminal Ulcer – A 2016 Update
Sunday, October 23rd, 2016
2016
In April 2016, the National Pressure Ulcer Advisory Panel or NPUAP announced a change in the terminology and the stages of pressure injuries. Though these stages continue to include both unstageable pressure injuries and deep tissue pressure injuries the new definitions do not specifically mention the Kennedy Terminal Ulcer. Over the years, however, multiple panels and advisory groups have documented the Kennedy Ulcer as an end of life phenomenon.
The unavoidable skin breakdown that occurs as part of the dying process, known as a Kennedy Ulcer, has been recognized by Ostomy Wound Management since a 2009 journal article. Also in 2009, an expert panel released a consensus statement known as SCALE or Skin Changes At Life’s End which identified skin organ compromise occurring at the end of life. The panel recognized that the ulcer is usually seen on the coccyx or sacrum but has been reported in other anatomical areas and is usually associated with imminent death.
This special classification was also mentioned by the Center for Medicare and Medicaid Services (CMS) in 2014 within its Quality Reporting Program Manual and its Continuity Assessment Record and Evaluations Data Set (CARE) for long-term care hospitals. The “Coding Tips” of the publication noted if an ulcer was part of the dying process, developing from six weeks to two to three days before death, it should not be coded as a pressure ulcer.
Click here for the full detailed staging guidelines.
ALN Consulting will continue to stay on top of these and other developments. Contact ALN Consulting if you have questions about a case and would like an initial consultation.
2015
This portion originally published on October 26, 2015:
It is well known that a pressure ulcer is an area of skin that breaks down when pressure on the skin reduces blood flow to the area. However, the knowledge and acceptance of skin failure at the end of life from various etiologies, including the Kennedy Terminal Ulcer (KTU), is growing among evidence based practitioners. The Kennedy Terminal Ulcer and other unavoidable similar skin phenomenon such as Skin Failure, SCALE (Skin Changes at Life’s End), Deep Tissue Injury (DTI), and the Tremblay-Brennan Terminal Tissue Injury were addressed at the most recent VCU Pressure Ulcer Summit by experts and scholars in the field.
The Kennedy Terminal Ulcer was first described by Karen Lou Kennedy in 1989, and evidence of poor perfusion to the skin causing a pressure ulcer-like damage of soft tissue in serious illness and at the end of life is well documented. While there are several etiologies that could cause unavoidable skin failure, the Kennedy Terminal Ulcer is focused on soft tissue injury on bony prominences, usually on the sacrum, during the dying process.
As illustrated in the photos, the Kennedy Terminal Ulcer has a sudden onset of a purple/red blister or abrasion, and rapidly progresses to a Stage III or IV ulcer. While further research is required, and was recommended by the PU Summit, there is general consensus that if a dying patient has blood perfusion issues that affect many other organs, known as multi-organ failure, then it is reasonable to accept that the lack of blood perfusion also can affect the skin resulting in unavoidable soft tissue injuries, despite adequate prevention measures.

Kennedy Terminal Ulcer

A phenomenon called “3:30 Syndrome” presented as a subdivision of the Kennedy Terminal Ulcer, which forms more quickly and appears as black spots.
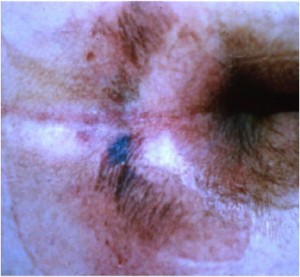
The classic “butterfly” or “horseshoe” shape of the Kennedy Terminal Ulcer.
In the near future the ANCC Magnet commissioners plan to develop and create access to a Magnet Designated Facility Database for hospital acquired pressure ulcers (HAPU) to promote ongoing research for unavoidable pressure ulcers and uncharacteristic soft tissue injuries that occur despite appropriate implementation and escalation of interventions to prevent skin injury and ulcers at the end of life.
References
- Brindle, Creehan, Black, & Zimmerman. (2015). The VCU Pressure Ulcer Summit: Collaboration to Operationalize Hospital-Acquired Pressure Ulcer Prevention Best Practice Recommendations. J Wound Ostomy Continence Nursing, 2015:00(0):1-7.
- Kennedy-Evans, Karen. (2012). The Life and Death of the Skin. [Nursing Home/ALF Litigation Seminar].
- Kennedy Terminal Ulcer. (2014). Retrieved October 7, 2015, from Kennedy Terminal Ulcer web site: http://www.kennedyterminalulcer.com/
Measuring Pain and Suffering
Monday, October 17th, 2016
It doesn’t take an attorney to know that pain and suffering go beyond an initial physical injury. Mental pain and suffering often ranges from lack of sleep or energy to humiliation, hypervigilance, consuming anger, mood swings, sexual dysfunction, and even PTSD (Post-Traumatic Stress Disorder). In a nutshell, an accident or injury can impact someone’s enjoyment of life. Plaintiff attorneys must quantify not only the physical and mental pain and discomfort a client has already experienced, but also what an expert can reasonably predict in the future.
A comparatively minor accident has far-reaching ramifications of which a judge or jury may not conceive. A pedestrian with the right-of-way can be hit in the crosswalk by a car, but ultimately walk out of an emergency room without broken bones or significant physical trauma. But a diagnosis of soft tissue damage doesn’t spell out that the person has been unable to sit without pain for a year. It doesn’t convey that he or she experienced nightmares for weeks, feared crossing streets for months, or was unproductive due to physical pain and an erratic sleeping pattern.
Even if a victim’s livelihood doesn’t involve significant physical labor, pain and discomfort find their way into a daily work life. Moving around with pain in what seems like an undemanding job can slow a person down. A part-time administrative professional can be laid off for cutting hours back to attend physical therapy…and be forced to hunt for a new job in between doctor’s appointments and pain that doesn’t follow a schedule.
For that hypothetical pedestrian, consequences like these were caused by the defendant. That pedestrian is entitled to compensation for all of the consequences – particularly, the mental or financial effects that remain long after the bones have healed and the bruises have disappeared. The law even recognizes mental pain and suffering of a less catastrophic nature – such as being unhappy about missing a family wedding because of post-incident physical limitations or pain. But the less obvious the effects, the greater the onus on the plaintiff to prove that the amount of damages sought are reasonable.
There are palpable odds stacked against anyone who seeks legal relief for pain and suffering. Negligence claims require a solid establishment of causation between the defendant’s actions and the negative effects on a plaintiff’s life. Plaintiff attorneys should establish that the client took reasonable steps to minimize or mitigate damages done, including seeking medical attention in a timely manner. Compensation can be reduced if he or she can even be considered partially responsible for an accident. Even a legitimate delay in diagnosis or treatment can hurt a case.
Along with the letter of the law, plaintiffs are up against juries with limited, subjective knowledge. In general, juries are not offered concrete guidelines for quantifying the value of pain and suffering. Mostly they use their common sense and personal background – which is highly variable and colored by personal opinions.
And like members of a jury, plaintiffs come out of the general population. A witness with limited communication skills may not be able to fully and accurately convey the mental or physical effects. It is also challenging to measure the pain and suffering of an accident victim who is not alive to testify on his or her own behalf. A plaintiff’s likeability and credibility can sway jury opinions.
The litigious society we live in makes it all the more important for a professional with a specific skill set to review and explain the physical and mental repercussions of an incident. Plaintiffs need as much solid evidence as possible to counteract a jury’s skepticism. And yet an endless string of witnesses and extensive medical records can overwhelm and confuse a jury more than edify them.
Documenting Pain And Suffering
That’s why it behooves a plaintiff to request a separate pain and suffering report. Also known as a FRE 1006 summary witness report, this is a special request that can be completed by a legal nurse consultant (LNC). Evaluating non-economic, non-concrete damages takes special expertise that someone with both legal and medical acumen can offer. An LNC can review complex, extensive medical records and summarize pain and suffering in ways that laypeople in a jury box can relate.
On one hand, this report humanizes the suffering victim in a way that a diagnosis can’t translate. On the other hand, a clearly detailed report in clinical terms can document how the subject’s life has changed as a result of someone else’s mistake.
At the end of the day, in fact, pain and suffering is often a repercussion of someone else’s poor decisions. By treating it with the same consideration as high blood pressure, for example, a plaintiff’s legal team can move closer to achieving a fair and reasonable settlement for a client.
Strengthen your case with a FRE 1006 summary witness report from ALN Consulting.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.