Posts Tagged ‘Attorney Knowledge Update’
Kennedy Terminal Ulcer – A 2016 Update
Sunday, October 23rd, 2016
2016
In April 2016, the National Pressure Ulcer Advisory Panel or NPUAP announced a change in the terminology and the stages of pressure injuries. Though these stages continue to include both unstageable pressure injuries and deep tissue pressure injuries the new definitions do not specifically mention the Kennedy Terminal Ulcer. Over the years, however, multiple panels and advisory groups have documented the Kennedy Ulcer as an end of life phenomenon.
The unavoidable skin breakdown that occurs as part of the dying process, known as a Kennedy Ulcer, has been recognized by Ostomy Wound Management since a 2009 journal article. Also in 2009, an expert panel released a consensus statement known as SCALE or Skin Changes At Life’s End which identified skin organ compromise occurring at the end of life. The panel recognized that the ulcer is usually seen on the coccyx or sacrum but has been reported in other anatomical areas and is usually associated with imminent death.
This special classification was also mentioned by the Center for Medicare and Medicaid Services (CMS) in 2014 within its Quality Reporting Program Manual and its Continuity Assessment Record and Evaluations Data Set (CARE) for long-term care hospitals. The “Coding Tips” of the publication noted if an ulcer was part of the dying process, developing from six weeks to two to three days before death, it should not be coded as a pressure ulcer.
Click here for the full detailed staging guidelines.
ALN Consulting will continue to stay on top of these and other developments. Contact ALN Consulting if you have questions about a case and would like an initial consultation.
2015
This portion originally published on October 26, 2015:
It is well known that a pressure ulcer is an area of skin that breaks down when pressure on the skin reduces blood flow to the area. However, the knowledge and acceptance of skin failure at the end of life from various etiologies, including the Kennedy Terminal Ulcer (KTU), is growing among evidence based practitioners. The Kennedy Terminal Ulcer and other unavoidable similar skin phenomenon such as Skin Failure, SCALE (Skin Changes at Life’s End), Deep Tissue Injury (DTI), and the Tremblay-Brennan Terminal Tissue Injury were addressed at the most recent VCU Pressure Ulcer Summit by experts and scholars in the field.
The Kennedy Terminal Ulcer was first described by Karen Lou Kennedy in 1989, and evidence of poor perfusion to the skin causing a pressure ulcer-like damage of soft tissue in serious illness and at the end of life is well documented. While there are several etiologies that could cause unavoidable skin failure, the Kennedy Terminal Ulcer is focused on soft tissue injury on bony prominences, usually on the sacrum, during the dying process.
As illustrated in the photos, the Kennedy Terminal Ulcer has a sudden onset of a purple/red blister or abrasion, and rapidly progresses to a Stage III or IV ulcer. While further research is required, and was recommended by the PU Summit, there is general consensus that if a dying patient has blood perfusion issues that affect many other organs, known as multi-organ failure, then it is reasonable to accept that the lack of blood perfusion also can affect the skin resulting in unavoidable soft tissue injuries, despite adequate prevention measures.

Kennedy Terminal Ulcer

A phenomenon called “3:30 Syndrome” presented as a subdivision of the Kennedy Terminal Ulcer, which forms more quickly and appears as black spots.
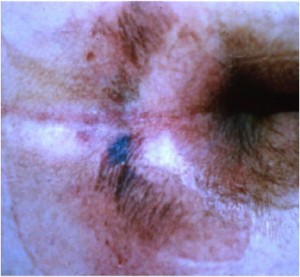
The classic “butterfly” or “horseshoe” shape of the Kennedy Terminal Ulcer.
In the near future the ANCC Magnet commissioners plan to develop and create access to a Magnet Designated Facility Database for hospital acquired pressure ulcers (HAPU) to promote ongoing research for unavoidable pressure ulcers and uncharacteristic soft tissue injuries that occur despite appropriate implementation and escalation of interventions to prevent skin injury and ulcers at the end of life.
References
- Brindle, Creehan, Black, & Zimmerman. (2015). The VCU Pressure Ulcer Summit: Collaboration to Operationalize Hospital-Acquired Pressure Ulcer Prevention Best Practice Recommendations. J Wound Ostomy Continence Nursing, 2015:00(0):1-7.
- Kennedy-Evans, Karen. (2012). The Life and Death of the Skin. [Nursing Home/ALF Litigation Seminar].
- Kennedy Terminal Ulcer. (2014). Retrieved October 7, 2015, from Kennedy Terminal Ulcer web site: http://www.kennedyterminalulcer.com/
Prevention and Policy: Falls in Long Term Care
Thursday, December 10th, 2015
The World Health Organization (WHO) defined falls in the 2007 Global Report on Falls Prevention in Older Age as, “inadvertently coming to rest on the ground, floor or other lower level, excluding intentional change in position to rest in furniture, wall or other objects.” The definition of falls does not include injury because not all falls cause injury. In fact, the CDC reports that one out of three older people fall each year, but less than half tell their doctor. Falling once doubles the chance of another fall. Insurance carrier actuarial analysis from 2014 showed that long term care liability claims are rising 3% annually, and falls are the most frequent allegation from skilled nursing facilities. On average, the claims had total payments of $131,104-171,960. Beyond consideration of the monetary losses of the facility, falls also have a major impact both physically and psychologically on those injured. Furthermore, the CDC reports that there were 25,464 deaths in 2013 from unintentional falls in the over 65 population in the United States, and falls are the most common cause of hip fractures and traumatic brain injuries. Falls should be among a long term care facility’s top priorities in terms of prevention and policy review.
The dichotomy which exists in long term care fall prevention is in the value placed on quality of life and autonomy where possible, and treatment goals to maximize mobility and minimize restraint. Long term facilities exist not just to prevent injury, but also provide a home for the resident, where the staff attempts to balance safety and precaution with the desires and autonomy of the resident. Janice Morse RN, PhD, the creator of a well-known fall risk assessment tool, the “Morse Fall Scale,” acknowledged as far back as 1987 that not all falls are preventable, and grouped falls into three types: physiological anticipated, physiological unanticipated, and accidental falls. Morse felt that even though some falls may not be preventable, the goal of the interdisciplinary team should still be to do all they could in prevention, and many of the risk strategies that she and her team published in 1987 still stand today as the standard of fall prevention care.
Risk Assessment
While there are many fall risk assessment and screening tools used throughout the U.S., three tools have been validated in multiple studies: The St. Thomas’ Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY), the Morse Falls Scale, and the Hendrich II Fall Risk Model. It is the standard of care to assess a resident for risk of falls upon admission, and re-evaluate risk upon change in resident condition. Issues which can raise a resident’s risk of falling include:
- History of falls.
- Medications (anti-cholinergics, anti-epileptics, antipsychotics, anti-hypertensives, antihistamines, benzodiazepines, sedative hypnotics, and recent changes in medication regimens).
- Co-morbidities such as osteoporosis, incontinence, cardiovascular disease, and pain.
- Vision changes.
- Decreased strength and mobility.
- Activity of Daily Living (ADL) assistance needs.
- Diabetes (blood sugar irregularities, peripheral neuropathy).
It seems the more of these risk factors a resident has, the more synergistic the risk factors become causing a much higher risk of falls in residents with multiple risk factors. In addition to the skilled nursing facility staff assessing the resident’s risk, the family should be involved in ensuring they have a clear picture of the resident’s health and have realistic expectations of the risks involved if their loved one does not comply with using the call bell and other preventative measures instituted. Keeping the family informed and part of the planning process many times contributes positively to the outcome should a fall occur.
Prevention
It is not enough to merely identify risk. Once risk has been assessed, resident specific interventions should be identified and implemented. Each resident should have a plan of care which addresses falls and injury risk. Dr. Craig Wilson, in a recent presentation on Fall Prevention, recommended the following universal fall reduction strategies (instituted regardless of fall risk) for all residents:
- Orient new residents to the environment, and instruct residents on the proper use of the nurse call system, ensuring they are operational and accessible for all residents.
- Position important items such as call light, water, and telephone within reach.
- Maintain an obstruction/spill-free environment.
- Remove all electrical cords from traffic areas.
- Place the bed in the lowest position with brakes locked.
- Use non-skid socks or footwear when out of bed.
- Utilize nightlights during evening shifts.
- Reassess ambulation status daily.
- Note and report changes in physical and mental status promptly.
- Never leave a resident unattended in the bathroom.
According to geriatric falls expert Elizabeth Hill, RN, PhD, studies have shown that individuals are at greater risk of falling when they are in the process of performing purposeful actions such as reaching for an object or using the toilet. Therefore, some of the most important interventions your facility can incorporate is the proper use of assistive devices such as grabbers and shoe horns, and hourly rounding. Hourly rounding is not the standard, most long term facilities check on residents at least every two hours, but rounding more often can eliminate many of the falls associated with non-compliance with the call system. Ms. Hill describes the “4 P’s” included in a nursing staff check, which include: Pain, Potty, Positioning, and Possessions.
Other important prevention categories include monitoring devices, such as bed alarms and surveillance, bed rails use to the extent that it assists residents with bed mobility but does not restrain free movement, keeping the bed in a locked and low position, and use of floor mats, larger mattresses, and hip protectors. Use of the interdisciplinary team beyond nursing, such as CNA’s, Occupational Therapy, Physical Therapy, Pharmacists, and Podiatrists can cover many of the reassessment points needed for a comprehensive plan that is continually updated based on resident condition and changes.
Response to Falls to Improve Outcomes and Minimize Risk
Let’s say your facility had a comprehensive and accurate assessment of a new resident, and created and implemented a care plan that was felt to be complete by the entire interdisciplinary team, and yet the resident still sustained a fall with possible injury. What are the immediate important steps for your staff to take? The first steps should focus on the resident’s safety:
- Evaluate level of consciousness and vital signs.
- Ask the resident if there is any neck or back pain, and assess pain all over the body.
- Check the skin for bruising, or injury.
- Notify the doctor, supervisor, and family (the doctor should always be notified before the family and documented as such). Determine with the physician if the resident needs to be transferred to the ED for further evaluation and treatment.
- If the resident stays in the facility, monitor neurological checks for at least 24 hours for unwitnessed falls.
All of the immediate steps should be documented comprehensively, and actions should be timely and documented as such.
Once the resident’s immediate safety is addressed and documented, and all appropriate actions are taken, an investigation should be done. A root cause analysis should be performed, and all plans should be reassessed and tailored to the resident’s new status. If the resident sustained a reportable injury it should be communicated to the State Board of Health. The family should be involved in new strategies for falls prevention.
Policy and Prevention of Litigation
Above all, a facility must have a falls policy in place that is frequently reviewed and updated. New staff should have a set training program for education regarding falls, and each unintentional fall should have a pathway for treatment and documentation that is practiced. The implementation of a “Falls Team” or IDT who reviews each fall, performs root cause analysis, and ensures implementation of new interventions for prevention is not a “standard of care” per se, but is a best practice and can decrease risk in your facility. Should you find your facility in the unfortunate position of defending a fall/injury case, a legal nurse consultant will help the legal team identify strengths and weaknesses in the assessment, prevention, and treatment rendered. If your facility and all its staff are committed to keeping falls from occurring in the long term setting, and continually work to implement interventions based on the residents’ current condition, you will have a low risk of litigation from falls and injury.
References
1. World Health Organization. (2007). WHO Global Report on Falls Prevention in Older Age. Retrieved October 16, 2015 from the World Health Organization website: http://www.who.int/ageing/publications/Falls_prevention7March.pdf
2. Aon 2014 Long Term Care Liability Actuarial Analysis. http://www.phca.org/docs/Aon_2014_Long_Term_Care_Liability_Actuarial_Analysis_full.pdf.
3. AON 2011 General Liability and Professional Liability Actuarial Analysis. http://www.aon.com/risk-services/thoughtleadership/reports-pubs_2011_long_term_care_survey.jsp
4. CNA Aging Services Report 2012 https://www.cna.com/vcm_content/CNA/internet/Static%20File%20for%20 Download/Risk%20Control/Medical%20Services/AgingServices2012DataAnalysis-SupportingtheNeedforIndustryChange-10-2012.pdf.
5. Falls among Older Adults: An Overview. Centers for Disease Control and Prevention. http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html.
6. MMWR QuickStats: Death Rates* from Unintentional Falls† Among Adults Aged ≥65 Years, by Sex — United States, 2000–2013. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6416a12.htm.
7. Morse, J.M., Tylko, S.J., & Dixon, H.A. (1987). Characteristics of the fall-prone patient. Gerontologist, 27(4), 516-522.
8. Oliver D et al. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997 Oct 25; 315(7115):1049-53.
9. Morse JM et al. A prospective study to identify the fall-prone patient. Soc Sci Med. 1989; 28(1):81-6.
10. Hendrich AL et al. Validation of the Hendrich II Fall Risk Model: a large concurrent case/control study of hospitalized patients. Appl Nurs Res. 2003 Feb; 16(1):9-21.
11. Meade, C.M., Bursell, A.L., & Ketelson, L. (2006). Effects of nursing rounds: on patients’ call light use, satisfaction, and safety. American Journal of Nursing, 106(9), 58-70.
12. Bloom, A.S. (2015). Back to Basics: Falls, Wounds, Infection and Death. [DRI Presentation].
13. Wilson, C.J. (2015). Don’t Get Tripped Up: State of the Art Fall Prevention. [DRI Presentation].
14. Hill, Elizabeth (2015). The Latest in Falls and Fall Prevention. [DRI Presentation].
Pressure Ulcer 2016 Update: Strategies to Defend Against Medical Malpractice Claims
Wednesday, November 18th, 2015
2016
In April 2016, the National Pressure Ulcer Advisory Panel or NPUAP announced a change in the terminology and the stages of pressure injuries. Though these stages continue to include both unstageable pressure injuries and deep tissue pressure injuries the new definitions do not specifically mention the Kennedy Terminal Ulcer. Over the years, however, multiple panels and advisory groups have documented the Kennedy Ulcer as an end of life phenomenon.
The unavoidable skin breakdown that occurs as part of the dying process, known as a Kennedy Ulcer, has been recognized by Ostomy Wound Management since a 2009 journal article. Also in 2009, an expert panel released a consensus statement known as SCALE or Skin Changes At Life’s End which identified skin organ compromise occurring at the end of life. The panel recognized that the ulcer is usually seen on the coccyx or sacrum but has been reported in other anatomical areas and is usually associated with imminent death.
This special classification was also mentioned by the Center for Medicare and Medicaid Services (CMS) in 2014 within its Quality Reporting Program Manual and its Continuity Assessment Record and Evaluations Data Set (CARE) for long-term care hospitals. The “Coding Tips” of the publication noted if an ulcer was part of the dying process, developing from six weeks to two to three days before death, it should not be coded as a pressure ulcer.
Click here for the full detailed staging guidelines.
ALN Consulting will continue to stay on top of these and other developments. Contact ALN Consulting if you have questions about a case and would like an initial consultation.
A thorough understanding of the development and treatment of pressure ulcers is critical when defending against these medical malpractice cases. Attorneys must stay up-to-date with the latest definitions, risk factors, and stages of pressure ulcers to help address the complicated claims in these cases. Studying the prevention and treatment of pressure ulcers allows for the strongest defense to be made. Pressure ulcer cases are rarely straightforward. Growing debate around the avoidability of pressure ulcers gives more room for defense teams to make defensible claims.
This portion originally published on November 18, 2015:
What is a Decubitus or Pressure Ulcer?
The term decubitus ulcer (from Latin decumbere, “to lie down”), pressure sore, bed sore, and pressure ulcer are often used interchangeably among patients, family, and medical staff. As the root of the name suggests, these ulcers occur at sites overlying bony structures that sustain more pressure when the person is recumbent. The National Pressure Ulcer Advisory Panel (NPUAP) and the most up to date literature refer to these type of ulcers as pressure ulcers, or an area of unrelieved pressure over a defined area, usually over a bony prominence, resulting in ischemia, cell death, and tissue necrosis.
Risk Factors for Pressure Ulcers
In a Long Term Care (LTC) setting surveyors follow the guidelines of F-tag #F314 which states that an admission assessment must be performed, along with an identification of patients who are at risk for pressure ulcers. There is no one formal risk assessment tool recommended, but many facilities use the Norton or Braden scales. Risk factors mentioned in #F314 include, but are not limited to:
- Impaired/decreased mobility and decreased functional ability;
- Co-morbid conditions, such as end stage renal disease, thyroid disease or diabetes;
- Drugs such as steroids that may affect wound healing;
- Impaired diffuse or localized blood flow;
- Resident refusal of some aspects of care and treatment;
- Cognitive impairment;
- Exposure of skin to urinary and fecal incontinence;
- Under nutrition, malnutrition, and hydration deficits;
- A healed ulcer. The history of a healed pressure ulcer and its stage (if known) is important since areas of healed Stage III and IV pressure ulcers are more likely to have recurrent skin breakdown; and
- Diabetic neuropathy, frailty, cognitive impairment.
Regardless of any individual’s risk score, the nursing staff is responsible for the creation of a resident specific care plan that addresses each risk factor and the extent to which the factors can be modified, stabilized or removed.
Staging of Pressure Ulcers
An important facet of caring for a patient with pressure ulcers is assessment and re-assessment of the stage, size, and appearance. If a pressure ulcer exists upon admission, or develops during residency, the stage of the ulcer should be documented. Nursing staff should not use the following staging system for ulcers that are not a result of pressure, such as ulcers and wounds called arterial ulcers (the result of blockage in the arteries with inadequate blood flow to the limbs), venous insufficiency ulcers (known as “stasis ulcers”), and diabetic ulcers. These ulcers should be documented, reported to the physician, and monitored, but not staged using the NPUAP International Classification System. For use along with the below NPUAP definitions of each stage, artistic renditions of the skin layers of these stages, as well as pictures for reference can be found at: http://www.npuap.org/wp-content/uploads/2014/08/Updated-10-16-14-Quick-Reference-Guide-DIGITAL-NPUAP-EPUAP-PPPIA-16Oct2014.pdf
 Stage I: Nonblanchable Erythema: Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin many not have visible blanching; its color may differ from the surrounding area.
Stage I: Nonblanchable Erythema: Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin many not have visible blanching; its color may differ from the surrounding area.
The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Stage I may be difficult to detect in individuals with dark skin tones. May indicate “at risk” individuals (a heralding sign of risk).
Stage II: Partial Thickness Skin Loss: Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled blister.
Presents as a shiny or dry shallow ulcer without slough or bruising. ⃰ Stage II should not be used to describe skin tears, tape burns, perineal dermatitis, maceration or excoriation.
 Stage III: Full Thickness Skin Loss: Full thickness loss of tissue. Subcutaneous fat may be visible, but bone, tendon, or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling.
Stage III: Full Thickness Skin Loss: Full thickness loss of tissue. Subcutaneous fat may be visible, but bone, tendon, or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling.
The depth of a Stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and a Stage III can be shallow. In contrast, areas of significant adiposity can develop extremely deep Stage III pressure ulcers. Bone/tendon is not visible or directly palpable.
 Stage IV: Full Thickness Tissue Loss: Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling.
Stage IV: Full Thickness Tissue Loss: Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling.
The depth of a Stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e.g. fascia, tendon or joint capsule) making osteomyelitis possible. Exposed bone/tendon is visible or directly palpable.
 Unstageable: Depth Unknown: Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed.
Unstageable: Depth Unknown: Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed.
Until enough slough and/or eschar is removed to expose the base of the wound, the true depth, and therefore stage, cannot be determined. Stable (dry, adherent, intact without erythema or fluctuance) eschar on the heels serves as ‘the body’s natural (biological) cover’ and should not be removed.
Suspected Deep Tissue Injury (SDTI): Depth Unknown: Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue.
Deep tissue injury may be difficult to detect in individuals with dark skin tones. Evolution may include a thin blister over a dark wound bed. The wound may further evolve and become covered by thin eschar. Evolution may be rapid exposing additional layers of tissue even with optimal treatment.
On April 8, 2016, the NPUAP will hold the 2016 Staging Consensus Conference at the Hilton Rosemont/Chicago O’Hare Hotel. Attendees will have the unique opportunity to provide input on the future of the staging system as it is now, including the possibility of doing away with the staging system altogether. Find out more here: http://www.npuap.org/events/2016-staging-consensus-conference/
Prevention Strategies
For prevention of pressure ulcer development, the 2014 NPUAP Quick Reference Guide recommends the following interventions (not an all-inclusive listing):
- Avoid positioning the individual on an area of erythema whenever possible.
- Keep the skin clean and dry.
- Do not massage or vigorously rub skin that is at risk of pressure ulcers.
- Develop and implement an individualized continence management plan.
- Protect the skin from exposure to excessive moisture with a barrier product.
- Consider using a skin moisturizer to hydrate dry skin in order to reduce risk of skin damage.
- Consider the need to control moisture and temperature when selecting a support surface.
- Do not apply heating devices directly on skin surfaces or pressure ulcers.
- Consider applying a polyurethane foam dressing to bony prominences.
- Assess the skin for signs of pressure ulcer development at each dressing change or at least daily. Use a finger or disc method to assess whether the skin is blanchable. A transparent disc is used to apply pressure equally over an area or erythema can help the nurse observe for blanching.
- Screen, assess and care plan for nutritional issues. Follow dietary requirements for offering or providing the correct amount of hydration, calories and protein. Keep in mind that “offer” or “provide” does not mean “consume” and no individual can be forced to eat or drink. If there is a risk of malnutrition or dehydration, alternatives should be provided to the individual and decision makers in the family (e.g. IV fluids, tube feedings).
- Reposition all individuals at risk of, or with existing pressure ulcers, unless contra-indicated. Consider a pressure redistribution support surface when determining the frequency of repositioning. (Other considerations when determining frequency are tissue tolerance, level of activity and mobility, general medical condition, overall treatment objectives, skin condition, and comfort).
- Document frequency, position, and outcome of repositioning plan.
- Teach individuals ‘pressure relief lifts’ or other pressure relieving maneuvers as appropriate.
- Add assessments of skin folds in obese individuals.
Most nurses are familiar with a standard of turning patients “Q2” or every 2 hours to prevent pressure ulcers. The current recommendations in the 2014 NPUAP Reference Guide do not prescribe a frequency that applies to every patient, but instead recommends that the staff take into account the above considerations and develop an individual plan based on the risk factors and patient condition.
Treatment Plans and Wound Healing
NPUAP treatment recommendations are based on scientific principles and the opinion of experts in the field. These recommendations include (but are not limited to):
- Complete comprehensive initial assessment and reassessment. Wound assessments should be documented, and deterioration should be addressed immediately. Existing pressure ulcers should be reassessed at least weekly.
- There should be some pressure ulcer healing within two weeks, with adjustment of expectations for healing in the presence of multiple factors that impair wound healing.
- Reevaluate the plan if the pressure ulcer does not show signs of healing within two weeks.
- Assess and treat pain.
- Cleanse the pressure ulcer and surrounding skin at the time of each dressing change. Cleanse with potable water or normal saline, or aseptic technique when the wound healing is compromised. Consider cleansing solutions with suspected or confirmed infection.
- Debride devitalized tissue within the wound bed or edge of pressure ulcers when appropriate, and when the presence of biofilm is confirmed or suspected. Do not debride stable, hard, dry eschar in ischemic limbs.
- Assess for and treat infection.
- Select a wound dressing based on the ability to keep the wound bed moist, need to address bacterial bioburden, nature and volume of wound exudate, condition of the tissue in the ulcer bed, condition of periulcer skin, ulcer size, depth, and location, presence of tunnelling and/or undermining, and goals of the individual with the ulcer.
- Use hydrocolloid dressings for clean Stage II pressure ulcers in body areas where they will not roll or melt.
- Use care in removing film dressings on fragile skin.
- Consider hydrogel dressings on shallow, minimally exuding pressure ulcers.
- Consider alginate dressings for the treatment of moderately and heavily exuding ulcers.
- Consider foam dressings on exuding Stage II and shallow Stage III ulcers.
- Consider silver-impregnated dressings for pressure ulcers that are clinically infected or heavily colonized but avoid prolonged use.
- Avoid gauze dressings for open pressure ulcers.
Avoidable vs. Unavoidable, and Defense of Pressure Ulcers
In the defense of pressure ulcer claims, a legal nurse consultant (LNC) can be the most important member of your defense team in sorting through the many and varied recommendations regarding pressure ulcers, especially in light of so many of the recommendations being suited to individualized care plans and the many factors of each individual patient. There are few “cut and dry” recommendations which apply universally.
In certain populations, the NPUAP and CMS have acknowledged that not all pressure ulcers are avoidable. The NPUAP defines an unavoidable pressure ulcer as “one that develops even though the provider has evaluated the patient’s clinical condition and pressure ulcer risk factors; defined and implemented preventive interventions consistent with the patient’s need and goals, and formulated with recognized standards of practice; monitored and evaluated the impact of the interventions; and revised care as appropriate.” F-tag #F314 describes an avoidable pressure ulcer as one that developed after the facility did not do one or more of the above interventions. Of particular interest to many in defense, is the growing literature and research backing the existence of unavoidable tissue injury or organ failure such as skin failure associated with the natural dying process. There are many terms which address such skin failure, such as SCALE (skin changes at life’s end), the Kennedy Terminal Ulcer (KTU), and Trombley-Brennan Terminal Tissue Injury. The VCU Pressure Ulcer Summit was held in March 2014 to redefine pressure ulcer prevention. The group agreed that most of these unavoidable ulcers at the end of life were not caused by pressure/shearing forces alone, and hypothesized they had underlying etiologies related to insufficient perfusion.
Important takeaways when defending a pressure ulcer case are:
- There are no “black and white” preventative and treatment measures. If the nursing staff regularly documents assessment and re-assessment, and tailors a plan which is implemented for each individual, as well as non-compliance by the patient in the treatment plan, this documentation can be the cornerstone of your defense.
- The patient may have diabetes which leads to “non-modifiable fixed deficits that can lead to non-preventable pressure ulcers.”
- Non-reversible peripheral neuropathy is a significant causative factor in development of pressure ulcers of the feet.
- Malnutrition present on admission can be a very high risk factor for pressure ulcer development.
- Incontinence of bowel and bladder requires dedication by nursing staff and can be complicated by medical problems such as C. diff and urinary tract infections.
- Obesity upon admission is a hurdle for facilities in many facets of health maintenance, especially in skin health. The barrier of noncompliance with nutritional dietary items, and the moisture involved in skin folds makes the obese patient a high risk for skin alteration.
- Arterial insufficiency can lead to amputations, but the misdiagnosis of an arterial ulcer for a pressure ulcer places an impossible preventative and treatment burden on the nursing staff. Without adequate blood flow to the limbs, and considering the treatments of elevation compression wraps adding to the pressure risk, this patient population is at high risk of unavoidable ulcers. Venous insufficiency can be clearly seen in most cases by lack of hair on lower extremities, with more darkly pigmented skin and edema. It complicates the management of pressure ulcers to a degree that is unrelated to the intervention given by nursing staff.
References
- Iyer, Patricia W. (2006). Nursing Home Liability and Its Consequences. In Nursing Home Litigation: Investigation and Case Preparation, 2nd (pp. 270-279). Tucson, AZ: Lawyers and Judges Publishing Co, Inc.
- Brindle, Creehan, Black, & Zimmerman. (2015). The VCU Pressure Ulcer Summit: Collaboration to Operationalize Hospital-Acquired Pressure Ulcer Prevention Best Practice Recommendations. J Wound Ostomy Continence Nursing, 2015:00(0):1-7.
- Haesler, Emily. (2014). National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Cambridge Media: Perth, Australia. Retrieved October 8, 2015
- Kirman, C., Geibel, J. (2015). Pressure Ulcers and Wound Care. Retrieved October 8, 2015 from Medscape web site.
- Lee, K. (2015). All the World’s a “Stage”: Pressure Ulcers – Prediction, Prevention and Treatment: A Review of the NPUAP 2014 Guidelines. [Presentation].
- Sharpe, J. N. (2015). Preventable vs. Non-Preventable Pressure Ulcers – Evaluation and Defense. [Presentation].

