Archive for the ‘Personal Injury’ Category
What the Mirena IUD Case Means for Expert Testimony
Monday, June 5th, 2017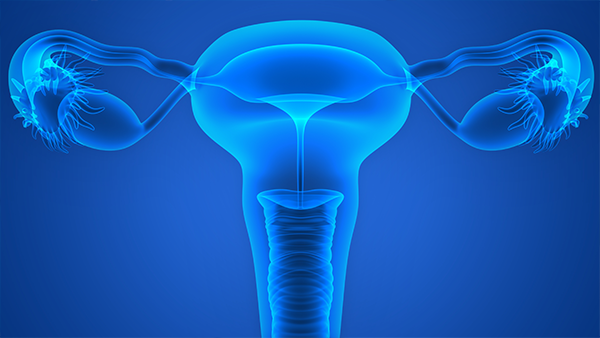
In 2011, the first personal injury complaint was made against Mirena, a plastic intrauterine device (IUD) used by over 2 million women worldwide. Manufactured by Bayer Healthcare Pharmaceuticals, one of the world’s largest pharmaceutical companies, Mirena is a T-shaped IUD coated with the hormone levonorgestrel. Designed to offer up to five years’ protection against unintended pregnancies, it is Bayer’s most popular IUD model and marketed as safe and effective.
Yet over a thousand women came forward alleging that Mirena can migrate once it is inserted into the uterus – perforating the uterus or cervix. Lawsuits allege that Bayer failed to adequately warn doctors and women about the risk of uterine perforation. Most of these women sued Bayer rather than their personal medical professionals. Their attorneys took the position that their medical side effects come from the IUD itself and not from an OB-GYN error in inserting the device.
The plaintiffs also claimed that Mirena’s label was misleading: it did not specify any necessary action other than having a doctor confirm the device’s placement. It only identified uterus perforation as a risk during the insertion, but not afterward. They allege that Bayer failed to warn patients of the risks associated with the IUD.
While marketing the drug, Bayer Healthcare sponsored “Mirena Parties” at which a nurse would make a scripted presentation on the benefits of using this IUD. Some plaintiffs claim that the different risks associated with its use were never elaborated upon. After these “parties” made their rounds, the FDA warned Bayer in writing that their marketing campaign was misrepresenting the issues with Mirena and to modify their advertising and presentations. This 2009 correspondence stated that the company had overstated Mirena’s efficiency, omitted information about its risk, and ultimately made a serious of false or misleading statements in its advertising.
Three years later, a study found that nearly half of doctors were not informed of the risks associated with the device. Bayer’s legal position, on the other hand, was that it was not aware of those side effects at the time of the marketing campaign and that they did not act irresponsibly.
Quality in expert witnesses
Expert witnesses were poised to testify that Mirena could cause uterine perforation after being inserted. The judge, however, found that these witnesses’ opinions were not supported by scientific literature and had been developed for the purpose of the lawsuit. In doing so, the defendants’ motion successfully barred these expert witnesses from even testifying.
Without established experts supporting their case, plaintiff attorneys countered that experts weren’t really needed to establish general causation. But the problem was that they had already named some to support their case. The court decided that it was well beyond the common understanding of lay jurors to discuss the uterus’s anatomy, the strength of its muscles, and the medical ramifications that could be caused by an IUD insertion procedure, and how existing technology could spot them. Thus, an expert on general causation testimony was not simply optional. So when plaintiff counsel claimed that the Mirena IUD lawsuits were “simple soft-tissue cases” that didn’t require expert opinions, their argument fell flat.
The plaintiffs also tried to argue that a series of purported party admissions of wrongdoing under 801(d)(2) could substitute for the required expert proof. The court, however, found that to substitute for expert testimony, it would have to be “the clearest and most unambiguous admission that the product or device in question can cause the alleged injury.” After walking through each case claiming a defendant admission, the plaintiff attorneys’ arguments still fell far short. Both individually and collectively, these admissions weren’t sufficiently clear, concrete, or detailed “to permit a jury to consider intelligently the existence, or not, of secondary perforation.”
The Mirena plaintiffs argued that the jury could and should assess what the defendants’ statements actually meant. But again, without expert testimony, a jury coming out of the general population could not be expected to have either the scientific or medical background to accurately evaluate these statements. They would speculate about whether a medical procedure could have caused the patients’ injuries, even though they had no information or training with which to make an informed decision.
This type of speculation is precisely why expert testimony is required. Without it, no jury would have a sound basis to find in favor of plaintiffs. The plaintiffs’ counsel had nothing to show they could carry their burden on general causation. A judgment was entered in favor of the defendant in all of the cases – all 1300 of them.
Legal nurse consultants: bridging the gap
How could things go so wrong for the plaintiffs when they had a damning FDA letter and study that supported their case? Clearly, drug and medical device causation calls for quality expert testimony that cannot be easily challenged in a court of law. And when it comes to medical negligence, so many health issues – both physical and emotional – are challenging to quantify.
Here is where a legal nurse consultant’s expertise is of particular value. Upon studying the files and medical records, this uniquely qualified consultant can formulate his or her own conclusions and recommend the right specialists for the case – from medical specialists to ancillary professionals like physical therapists and pharmacists. For a case like IUD negligence, an LNC would find an expert witness in obstetrics and gynecology. This OB-GYN would need to be familiar with the specific brand in order to explain that device’s specifics and any follow-up treatment. The LNC may also research literature and product issues relevant to the impending lawsuit.
With accusations of improper warnings, a legal nurse consultant can recruit a medical device labeling expert to explain the proper procedures and any existing warnings for the device. A mental health expert can best help lay jurors appreciate the full impact of the defendants’ error on the plaintiff’s life and well-being. Most importantly, both the LNC and the expert witnesses would convey both the causation and its consequences in terms that any member of the jury could understand.
While it is true that these professionals are hired to work for healthcare organizations as risk managers or risk reduction experts, they are also an enormous boon for mass torts and class action lawsuits, as well as individual suits. Legal nurse consultants are in a unique position to build the strongest, most manageable court case for their clients – and seek justice and relief for individuals who have suffered due to medical negligence.
Sources
- https://www.masstortnexus.com/mass-torts-news/federal-court-reopens-mirena-iud-product-liability-mdl/
- http://www.thenationaltriallawyers.org/2013/04/mass-tort-likely-over-mirena-iud-injuries/
- https://www.druganddevicelawblog.com/2016/08/summary-judgment-for-all-pending-cases-in-the-mirena-mdl.html
- https://www.theexpertinstitute.com/mirena-iud-a-mass-tort-primer/
- http://www.foxnews.com/health/2016/07/29/judge-rules-against-some-1300-lawsuits-over-bayers-mirena-iud.html
- http://www.youhavealawyer.com/mirena/
- https://www.law360.com/articles/792741/bayer-wants-all-mirena-iud-cases-tossed-for-lack-of-experts
- https://lawstreetmedia.com/issues/health-science/legal-battles-mirena-iud-whats-next/
Baby Powder Mass Tort Litigation: Strong Scientific Foundation or Just a Cloud of Dust?
Wednesday, April 26th, 2017
To first understand this subject, one needs to understand mass tort. You may have heard of a class-action lawsuit and associate the terminology with a mass tort lawsuit, but these are two separate types of cases despite implied similarities. Both types of cases involve a large number of individuals who claim to have been harmed by a common entity. The difference lies in procedurally how the plaintiffs are represented (Ashcraft and Gerel, LLP, n.d.). For class-action lawsuits, a firm files the lawsuit on behalf of all of those harmed, as one plaintiff with one trial; while for mass tort lawsuits, plaintiffs are treated individually, with separate trials (Rottenstein Law Group, LLP, n.d.). To proceed as a class action lawsuit, the Court must approve the claim as dictated by Rule 23 of the Federal Rules of Civil Procedure which states that:
- the class is so numerous that joinder of all members is impracticable;
- there are questions of law or fact common to the class;
- the claims or defenses of the representative parties are typical of the claims or defenses of the class; and
- the representative parties will fairly and adequately protect the interests of the class (Ashcraft and Gerel, LLP, n.d.).
If the Court does not approve the claim to proceed as a class action lawsuit, then the plaintiffs can individually proceed with mass tort litigation, each having their own trial in their own jurisdiction (Rottenstein Law Group, LLP, n.d.). In either case, firms may utilize mass media for advertisement to make the general public aware of possible harmful effects of a product or device. The firms may also use advertising to alert potential plaintiffs that claims are being filed, to gain more clients, and to make potential jurors aware, all in an indirect effort to gain victory.
In 2009, one of the first cases was filed, alleging that women’s genital use of talcum powder or baby powder has led to diagnoses of ovarian cancer, which in some cases, has proceeded to wrongful death.
One may ask, “how on earth can something applied to the outside of the body cause cancer in tissues located on the inside of the body?” The answers have taken years to prove, yet Cramer, Vitonis, Terry, Welch, and Titus (2016) explain that research on this very topic began back in the 1960’s, when there was the discovery that talcum powder contained asbestos—a current, well-known carcinogen (Cralley, Key, Groth, Lainhart, & Ligo, 1968; Graham & Graham, 1967). The group also explain the progression of scientific research demonstrating the link and cause of talcum/baby powder to ovarian cancers listing dozens of more studies. The literature review identifies specific risk factors and associations.
Essentially, the established facts are:
- Talc has fine particles which migrate through the vaginal canal, the cervical opening, the uterus and fallopian tubes to the ovaries, causing cellular changes predisposing a woman to cancer.
- The longer a woman has utilized genital-area application of talc (talc years), the more at-risk she is for cancer. There does not appear to be a correlation with the cornstarch variation of baby powder.
- There is an association between talc users and asthma; therefore, those who ended up with ovarian cancer also report having had a history of asthma.
- Other contributing factors point to an influence involving estrogen and/or prolactin in talc-users: pre-menopausal women, post-menopausal women who used hormone therapy, obese pre-menopausal women, and those who breastfed, currently smoke, or use alcohol.
- There seems to be a higher association among African American or Black women.
- The pathologic tissue subtypes of epithelial ovarian cancer which were more likely talc-associated, “include serous and mucinous borderline tumors and invasive serous and endometrioid tumors” (Cramer, Vitonis, Terry, Welch, & Titus, 2016, p. 345).
With mass tort litigation involving large numbers of plaintiffs, with vast medical histories and substantial medical records, it is crucial to utilize a staff which can efficiently organize, review, and analyzes the enormous associated files. It takes a group of professionals who are educated to assess and evaluate the case files for completeness, and who can perform critical thinking and analysis. The medical-legal professionals at ALN Consulting, perform this type of work, and more, every day. At ALN Consulting, we do more than help you prepare…we prepare you to win.
References
Ashcraft and Gerel, LLP. (n.d.). Class action vs. mass tort: a brief explanation [web page]. Retrieved from http://ashcraftandgerel.com/attorney-blogs/class-action-vs-mass-tort-a-brief-explanation/
Cralley, L. J., Key, M. M., Groth, D. H., Lainhart, W. S., & Ligo, R. M. (1968). Fibrous and mineral content of cosmetic talcum products. American Industrial Hygiene Association Journal, 29(4), 350-354.
Cramer, D. W., Vitonis, A. F., Terry, K. L., Welch, W. R. & Titus, L. J. (2016). The association between talc use and ovarian cancer: A retrospective case–control study in two US states. Epidemiology, 7(23), 334-346.
Graham, J., & Graham, R. (1967). Ovarian cancer and asbestos. Environmental Research, 1(2), 115-28.
Rottenstein Law Group, LLP. (n.d.) What is a “mass tort” [web page]. Retrieved from http://www.rotlaw.com/legal-library/mass-torts/
Measuring Pain and Suffering
Monday, October 17th, 2016
It doesn’t take an attorney to know that pain and suffering go beyond an initial physical injury. Mental pain and suffering often ranges from lack of sleep or energy to humiliation, hypervigilance, consuming anger, mood swings, sexual dysfunction, and even PTSD (Post-Traumatic Stress Disorder). In a nutshell, an accident or injury can impact someone’s enjoyment of life. Plaintiff attorneys must quantify not only the physical and mental pain and discomfort a client has already experienced, but also what an expert can reasonably predict in the future.
A comparatively minor accident has far-reaching ramifications of which a judge or jury may not conceive. A pedestrian with the right-of-way can be hit in the crosswalk by a car, but ultimately walk out of an emergency room without broken bones or significant physical trauma. But a diagnosis of soft tissue damage doesn’t spell out that the person has been unable to sit without pain for a year. It doesn’t convey that he or she experienced nightmares for weeks, feared crossing streets for months, or was unproductive due to physical pain and an erratic sleeping pattern.
Even if a victim’s livelihood doesn’t involve significant physical labor, pain and discomfort find their way into a daily work life. Moving around with pain in what seems like an undemanding job can slow a person down. A part-time administrative professional can be laid off for cutting hours back to attend physical therapy…and be forced to hunt for a new job in between doctor’s appointments and pain that doesn’t follow a schedule.
For that hypothetical pedestrian, consequences like these were caused by the defendant. That pedestrian is entitled to compensation for all of the consequences – particularly, the mental or financial effects that remain long after the bones have healed and the bruises have disappeared. The law even recognizes mental pain and suffering of a less catastrophic nature – such as being unhappy about missing a family wedding because of post-incident physical limitations or pain. But the less obvious the effects, the greater the onus on the plaintiff to prove that the amount of damages sought are reasonable.
There are palpable odds stacked against anyone who seeks legal relief for pain and suffering. Negligence claims require a solid establishment of causation between the defendant’s actions and the negative effects on a plaintiff’s life. Plaintiff attorneys should establish that the client took reasonable steps to minimize or mitigate damages done, including seeking medical attention in a timely manner. Compensation can be reduced if he or she can even be considered partially responsible for an accident. Even a legitimate delay in diagnosis or treatment can hurt a case.
Along with the letter of the law, plaintiffs are up against juries with limited, subjective knowledge. In general, juries are not offered concrete guidelines for quantifying the value of pain and suffering. Mostly they use their common sense and personal background – which is highly variable and colored by personal opinions.
And like members of a jury, plaintiffs come out of the general population. A witness with limited communication skills may not be able to fully and accurately convey the mental or physical effects. It is also challenging to measure the pain and suffering of an accident victim who is not alive to testify on his or her own behalf. A plaintiff’s likeability and credibility can sway jury opinions.
The litigious society we live in makes it all the more important for a professional with a specific skill set to review and explain the physical and mental repercussions of an incident. Plaintiffs need as much solid evidence as possible to counteract a jury’s skepticism. And yet an endless string of witnesses and extensive medical records can overwhelm and confuse a jury more than edify them.
Documenting Pain And Suffering
That’s why it behooves a plaintiff to request a separate pain and suffering report. Also known as a FRE 1006 summary witness report, this is a special request that can be completed by a legal nurse consultant (LNC). Evaluating non-economic, non-concrete damages takes special expertise that someone with both legal and medical acumen can offer. An LNC can review complex, extensive medical records and summarize pain and suffering in ways that laypeople in a jury box can relate.
On one hand, this report humanizes the suffering victim in a way that a diagnosis can’t translate. On the other hand, a clearly detailed report in clinical terms can document how the subject’s life has changed as a result of someone else’s mistake.
At the end of the day, in fact, pain and suffering is often a repercussion of someone else’s poor decisions. By treating it with the same consideration as high blood pressure, for example, a plaintiff’s legal team can move closer to achieving a fair and reasonable settlement for a client.
Strengthen your case with a FRE 1006 summary witness report from ALN Consulting.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.
National Pressure Ulcer Advisory Panel (NPUAP) Release New Clinical Guidelines and Taxonomy for Pressure Injuries
Friday, October 7th, 2016
In 1986, the National Pressure Ulcer Advisory Panel (NPUAP) was formed as an independent, non-profit organization established to ensure consistent prevention, management and research of pressure ulcers. Conflicts in research and prevention created the need for this governing body, an organization that would work to create guidelines and establish best practices surrounding pressure injury wounds. NPUAP serves as the authoritative voice for improved patient outcomes in pressure ulcer prevention and treatment through the development of public policy, education and research.
Subsequent to the formation of NPUAP, the terminology to describe “pressure ulcers” was redefined and the staging system of pressure wounds expanded. Although changes were made with the intent of clarifying the differences among the stages of pressure ulcers, the new classification system led to more confusion. For example, the use of the term “injury” and “ulcer” interchangeably caused great confusion.
In April 2016, a consensus conference was convened by NPUAP to review and revise the pressure injury staging system and to standardize the terminology used to describe injury to the skin from external pressure. The term “pressure ulcer” was changed to “pressure injury.” This simple change in terminology was actually monumental, as it was a major departure from the old taxonomy in the 30 years since the panel was formed. Updates to the panel’s description of the stages of pressure injuries were developed. The group indicated that the change in terminology would more accurately describe pressure injuries to both intact and ulcerated skin.
The 2016 definition of “Pressure injury” by NPUAP describes localized damage to the skin and underlying soft tissue usually over a bony prominence, related to a medical procedure such as prolonged surgery or from a medical device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shearing forces. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue. Shearing occurs from friction against the skin that leads to a superficial or partial thickness injury, often resembling an abrasion.
Pressure Injury Staging
The staging system further defined pressure injuries of stages 1-4 as well as including medical device related pressure injuries and mucosal membrane pressure injuries. The following illustrations denote each stage and classification of pressure injuries.
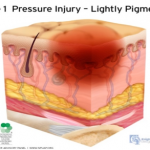 Stage 1 Pressure Injury: Non-blanchable erythema of intact skin. Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple of maroon discoloration; these may indicate deep pressure injury.
Stage 1 Pressure Injury: Non-blanchable erythema of intact skin. Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple of maroon discoloration; these may indicate deep pressure injury.
 Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible nor are deeper tissues. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible nor are deeper tissues. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
Stage 3 Pressure Injury: Full-thickness skin loss. Full thickness loss of skin, in which adipose tissue is visible in the ulcer, meets the definition of a Stage 3 pressure injury. Granulation tissue and epibole (rolled wound edges) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss, this becomes an Unstageable Pressure Injury.
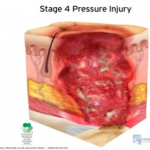 Stage 4 Pressure Injury: Full-thickness skin and tissue loss. Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole, undermining and/or tunneling often occur. The depth of the injury varies by anatomical location. If slough or eschar obscures the extent of tissue loss, an injury such as this would be described as an Unstageable Pressure Injury.
Stage 4 Pressure Injury: Full-thickness skin and tissue loss. Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole, undermining and/or tunneling often occur. The depth of the injury varies by anatomical location. If slough or eschar obscures the extent of tissue loss, an injury such as this would be described as an Unstageable Pressure Injury.
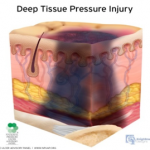 Deep Tissue Pressure Injury: persistent non-blanchable deep red, maroon or purple discoloration. This type of injury may involve either intact or non-intact skin, presenting with a localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss.
Deep Tissue Pressure Injury: persistent non-blanchable deep red, maroon or purple discoloration. This type of injury may involve either intact or non-intact skin, presenting with a localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss.
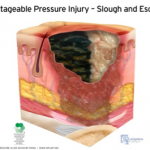
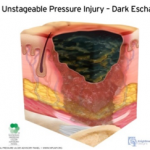 Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss. This type of injury involves full-thickness skin and tissue loss. The extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If the slough or eschar is removed from the wound, a stage 3 or stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss. This type of injury involves full-thickness skin and tissue loss. The extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If the slough or eschar is removed from the wound, a stage 3 or stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
As classifications and guidelines change, it’s critical to have an expert on your team who understands the current definitions. ALN Consulting’s team of legal nurse consultants have their finger on the pulse of these changes, and are trained to spot inaccuracies in medical records that can effect case outcomes. Contact ALN Consulting today to learn how we can help.
Identifying Medical Malpractice Expert Witnesses
Monday, June 6th, 2016
Sometimes medical negligence is apparent without need for explanation. It doesn’t take an expert to find fault when someone operates on the wrong limb or administers the wrong medication to a nursing home resident.
If medical professionals are the only ones with control over a negative outcome, and when an adverse event could only have been caused by a medical error, our legal system invokes the doctrine of res ipsa loquitur (Latin for “the thing speaks for itself.”) Simply stated, res ipsa is the principle noting that an event could have happened only due to negligence.
Although personal injury laws and rules of evidence are determined at the state level, the elements of res ipsa are pretty standard. For a case to meet the doctrine of res ipsa loquitur, three factors must be present: 1) the event would not occur in the absence of negligence; 2) the evidence of negligence rules out the possibility that the plaintiff’s actions caused the adverse event; and, 3) the negligent act occurs within the context of care provided by the defendant. It is often recommended that an expert witness be consulted, even in a case of res ipsa. The defendant’s attorney will usually challenge the notion that he or she had complete control over the circumstances.
In most cases of medical or nursing home negligence, expert witnesses are necessary to move a case forward. Lack of expert testimony can mean an early decision in an opponent’s favor – if not an outright dismissal. The facts and language of medicine are often too complex to understand. The appointed expert will walk the jury through the maze of medicine to understand why a lawsuit was filed in the first place.
Most states require plaintiffs to consult an expert witness to determine if the medical care provided to the plaintiff met the standard of care. In the legal arena, the standard of care is the level at which the average, prudent provider in a given community would practice. It is how similarly qualified practitioners would have managed the patient’s care under the same or similar circumstances. The standard of care is not necessarily the best care – just the average level expected of any care provider.
When a case does require qualified professional expertise, both plaintiffs and defendants must hire someone to serve in the role of expert witness. For cases to be tried in Federal Court, the Federal Rules of Civil Procedure (Fed.R. Civ.P.), requires the selected expert to prepare a detailed report in addition to a list of the expert’s prior testimony and compensation.
Although some states follow the Federal Rules of Civil Procedure, others have different rules for dealing with experts. In some states, an expert witness will be deposed before trial so the opposing side can be fully prepared to counter his or her opinions. In others, like New York, a legal team is not required to disclose the name of the designated expert, but they do have to provide opposing counsel with the expert’s bibliography.
What Makes A Medical Professional An Expert?
You may ask, “What makes a medical professional an expert?” One legal dictionary defines an expert as “a person who through education or experience has developed skill or knowledge in a particular subject so that he or she may form an opinion that will assist the fact finder.”
Each state has its own definition of who may be designated as a medical expert. Some states require that professional experience must be current, either for a specified number of years or that the expert was practicing in a clinical setting at the time of the incident. A degree from an AMA or AOA-accredited medical school are common requirements, as is board certification in the experts’ area of expertise. An unrestricted medical license with no recent history of suspension or revocation is paramount. Many states mandate that potential experts must devote a certain percentage of professional time to an active clinical practice, to avoid earning the reputation as a “professional witness.”
Nurse expert witnesses typically need a B.S.N. and recent clinical expertise in the same area as the defendant, with no record of legal issues or board disciplinary actions. Certification in the expert’s nursing specialty is an added plus.
Some states adhere to different versions of a specialty rule, which requires experts to practice in the same field of medicine as the defendant physician or nurse. A state’s locality rule obligates claimants to prove, by expert testimony, the recognized standard of acceptable professional practice in the community where the defendant medical provider practices or a similar community. For example, many states require that potential expert witnesses in medical malpractice cases must come from the state in which the alleged incident occurred or from a state contiguous to the venue in which the alleged incident occurred.
In most state malpractice lawsuits, attorneys on both sides will know the witnesses’ identities before getting to trial. They will research each expert’s career from their education to their publications. Every statement in an article written or testimony in cases with similar issues will be carefully scrutinized. The legal team will research the facts on which each claim is based – gleaning all it can to uncover the weak link in an expert’s opinion.
How Can An Expert Witness Be Utilized?
Expert witnesses can be used in a variety of ways. A medical professional may appear before the court as a “fact witness.” A “fact witness” is called to explain the medicine to the judge and jury. His or her role is to provide “just the facts” about a case, with no opinion regarding the medical care provided.
In medical malpractice and nursing home litigation, causation is the common Achilles’ heel. The rub lies in two questions every medical malpractice suit must answer. First, did the defendant fail to follow the standard of care for professionals in his or her position?
To answer this, a plaintiff-appointed expert may cite medical board guidelines or publications. What would industry standards expect of the defendant? How would a conscientious colleague with the same training treat this patient? What issues would that medical professional check for, and how would those issues be treated if diagnosed? An expert witness need not practice a higher standard of care than the defendant. He or she must only be conversant enough to determine that this standard was not followed.
The second question is thornier. If there was a breach in the standard of care, did this breach cause the negative outcome or damages? Given all the factors present, how likely was the plaintiff’s injury a result of substandard care?
The plaintiff’s goal is to find an expert who believes there is evidence of a breach of the standard of care. The defense will use its own expert to establish that the standard of care was observed – or that any deviation did not directly or proximately cause the adverse event. The plaintiff’s attorney, in turn, will get to work uncovering every possible way to challenge the defense’s expert testimony.
Finding properly credentialed healthcare professionals who are willing to offer opinions is not always easy. So what’s the best way to choose an expert witness? By consulting one.
Here is where a nurse’s expertise is of particular value. Upon studying the files and medical reports, this uniquely qualified consultant can recommend appropriate specialists.
Nursing expertise is ideal in complex cases of medical and care negligence. Identifying the probable cause of a medical event takes more than simply checking blood pressure and vital signs. A nurse is interested not only in physical agility but whether the patient has followed doctors’ and therapists’ directives and asked for assistance when necessary. This expert not only researches a patient’s diet, but whether or not the patient has adhered to the diet or eaten the food provided in a hospital or care facility. He or she would review physician progress notes, consultation reports, nursing progress notes, patient teaching records, lab results for specific issues and medication history for germane clues.
Legal nurse consultants (LNCs) are generally brought in to determine the merit of a case. Some help attorneys formulate questions to be asked at a deposition or trial. Some LNCs provide both consultation and testimony, while others prefer to work “behind the scenes.”
LNCs play a vital and advantageous role finding other experts for the case – from M.D. specialists to ancillary professionals like physical therapists, respiratory therapists, and pharmacists. Nurse expert witnesses are expected to testify at a deposition and trial if needed. Unlike the LNC consulting expert, the testifying expert may or may not be required to put their opinion in writing.
Both consulting LNCs and nurse expert witnesses review medical records and deposition testimony and formulate their conclusions. They commonly organize pertinent medical records and prepare record chronologies or timelines. They may also research medical and nursing literature and standards germane to issues in the suit brought forth. Both kinds of experts offer their own unique value to legal teams – and are often hired by healthcare organizations as risk managers or compliance experts.
As with other litigation, medical malpractice and long-term care cases often pit one expert against the other. Sometimes the tipping point in a jury’s decision is how well one witness can translate technical intricacies in to language they understand. ALN Consulting’s team of nurse consultants are in a unique position to build the strongest, most manageable court case for their clients – and boil medical-legal issues down to their essence. Contact us to learn how!
CMS Interpretive Guidelines – Revision to Feeding Tube Guidance
Wednesday, March 23rd, 2016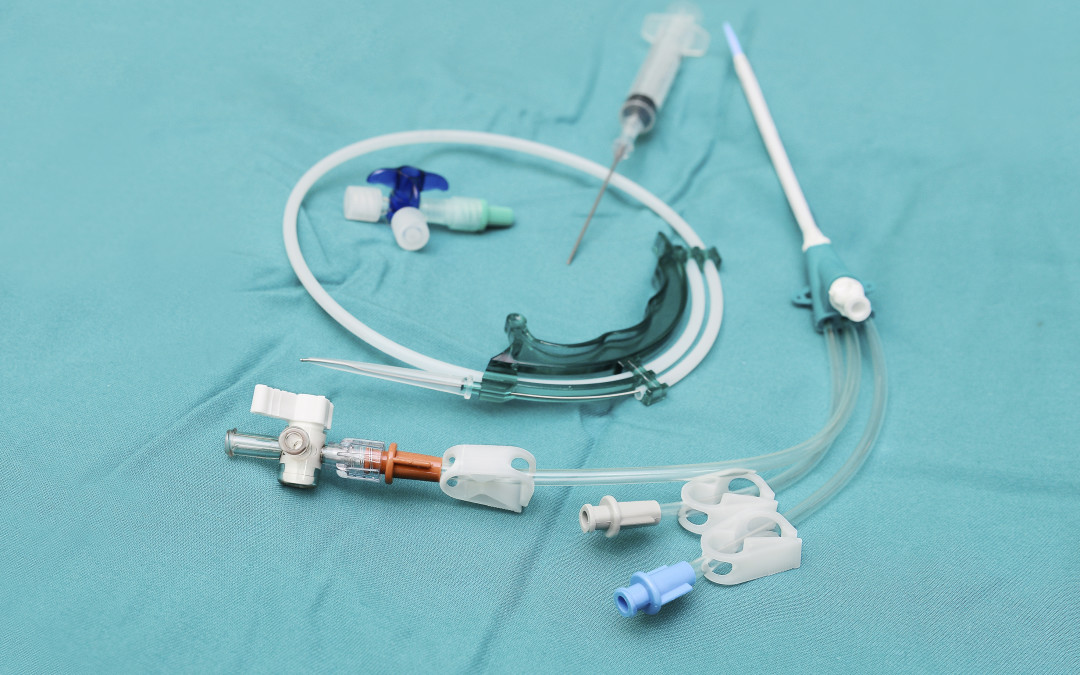
In this installment of the ALN Consulting series on the CMS Interpretive Guidelines, we explore the most recent revisions to surveyor guidance on feeding tubes in long-term care facilities. The Interpretive Guidelines include an explanation of the intent of the law, definitions of related terms, and instructions to surveyors on how to determine compliance with the law.
The CMS Interpretive Guidelines for Nasogastric tubes updates clarify expectations for long-term facility accountability in regards to use of feeding tubes; requiring that the resident’s legal representative be properly informed, specifying how nutritional needs are monitored, and mandating that potential risks associated with feeding tubes be considered in the decision making process.
The key to a strong defense against complaints related to long-term care residents’ nutritional status, particularly those who have feeding tubes, lies in a solid understanding of these guidelines and the recent revisions.
42 C.F.R. §483.25(g) Nasogastric Tubes (F tag 322)
The CFR Regulation states, “Based on the comprehensive assessment of a resident, the facility must ensure that:
- A resident who has been able to eat enough alone or with assistance is not fed by nasogastric tube unless the resident’s clinical condition demonstrates that use of a nasogastric tube was unavoidable; and
- A resident who is fed by a nasogastric or gastrostomy tube receives the appropriate treatment and services to prevent aspiration pneumonia, diarrhea, vomiting, dehydration, metabolic abnormalities, and nasal-pharyngeal ulcers and to restore, if possible, normal eating skills.”
Relevant definitions in the Interpretive Guidelines include:
Avoidable: There is not a clear indication for using a feeding tube, or there is insufficient evidence it provides a benefit that outweighs associated risks.
Unavoidable: There is a clear indication for using a feeding tube, or there is sufficient evidence it provides a benefit that outweighs associated risks.
Bolus feeding: The administration of a limited volume of enteral formula over brief periods of time.
Continuous feeding: The uninterrupted administration of enteral formula over extended periods of time.
Enteral nutrition (a.k.a. “tube feeding”): The delivery of nutrients through a feeding tube directly into the stomach, duodenum, or jejunum.
Feeding tube: A medical device used to provide enteral nutrition to a resident by bypassing oral intake.
Gastrostomy tube (“G-tube”): A tube that is placed directly into the stomach through an abdominal wall incision for administration of food, fluids, and medications. The most common type is a percutaneous endoscopic gastrostomy (PEG) tube.
Jejunostomy tube (a.k.a. “percutaneous endoscopic jejunostomy” (PEJ) or “J-tube”): A feeding tube placed directly into the small intestine.
Nasogastric feeding tube (“NG tube”): A tube that is passed through the nose and down through the nasopharynx and esophagus into the stomach.
Transgastric jejunal feeding tube (“G-J tube”): A feeding tube that is placed through the stomach into the jejunum and that has dual ports to access both the stomach and the small intestine.
Tube feeding (a.k.a. “enteral feeding”): The delivery of nutrients through a feeding tube directly into the stomach, duodenum, or jejunum.
Regulation Tag F 322
The feeding tube requirement has two parts. The first aspect requires that the facility utilize a feeding tube only after it determines that a resident’s clinical condition demonstrates this intervention was unavoidable. The second aspect requires that the facility provides to the resident who is fed by a tube services to prevent complications, to the extent possible, and services to restore normal eating skills, if possible.
The facility is in compliance with 42 CFR §483.25(g), if staff:
- Uses a feeding tube to provide nutrition and hydration only when the resident’s clinical condition makes this intervention necessary based on adequate assessment, and after other efforts to maintain or improve the resident’s nutritional status have failed;
- Manages all aspects of a feeding tube and enteral feeding consistent with current clinical standards of practice in order to meet the resident’s nutritional and hydration needs and prevent complications; and
- Identifies and addresses the potential risks and/or complications associated with feeding tubes, and provide treatment and services to restore, if possible, adequate oral intake.
Surveyor “Probes” in Facility Use of Feeding Tubes
Probes, or questions posed by the Interpretive Guidelines for surveyors, can be used by the defense team to bolster evidence that a practitioner or facility met the standard of care. There are many probes in F tag 322 related to resident rights; technical and nutritional aspects of feeding tubes; care of the feeding tube; and complications related to the feeding tube and/or the enteral nutrition product. Some examples of surveyor probes include:
- Was the resident and/or the resident’s legal representative informed about the relevant benefits and risks of tube feeding?
- How has the staff and practitioner determined the cause of decreased oral intake/weight loss or impaired nutrition and attempted to maintain oral intake prior to the insertion of a feeding tube?
- How did the staff determine the resident’s nutritional status was being met, such as periodically weighing the resident, and how did they decide whether the tube feeding was adequate to maintain acceptable nutrition parameters?
- How has the facility identified the resident at risk for impaired nutrition, identified and addressed causes of impaired nutrition, and determined that use of a feeding tube was unavoidable?
- How has the staff verified that the feeding tube was properly placed?
- How has the staff monitored a resident for possible complications (e.g., diarrhea, nutritional deficits, aspiration, depression, withdrawal, etc.) related to a feeding tube and the tube feeding, and how have they identified and addressed such complications?
Updates to the Interpretive Guidelines
The Interpretive Guidelines entitled Nasogastric tubes was vastly updated in November 2014. For the purpose of the guidelines, the regulatory title is considered to include any feeding tube used to provide enteral nutrition to a resident by bypassing oral intake. (Since the regulation was created use of actual nasogastric tubes have become rare, and use of other types of enteral feeding tubes have become more prominent.)
The newest guidance stresses the unavoidability standard, and also emphasizes quality of life and resident choice. Based on the guidelines, it could be argued that some examples of possible adverse effects from feeding tubes such as diminished socialization and loss of the experience of taste, texture, and chewing must be considered as important, and may possibly outweigh the benefits of feeding tubes such as preventing malnutrition and dehydration, and aiding wound healing. A new statement regarding the use of feeding tubes in elderly patients with dementia also addressed the controversy in this arena. “The literature regarding enteral feeding of these individuals suggests that there is little evidence that enteral feeding improves clinical outcomes (e.g., prevents aspiration or reduces mortality).”3
In the defense of the use, non-use, or complications of feeding tubes, the Interpretive Guidelines; Nasogastric tubes now provide a much larger framework for the difficult end of life decisions which are inherent in turning towards non-oral sustenance. With the comprehensive updates added to this guideline, ALN Consulting can help your defense team pinpoint crucial, relevant prompts and research to strengthen a case with complaints involving tube feeding.
References
- Harris, Rick E. (2015). How to Use the CMS Surveyor Guidance to Craft a Winning Defense [Presentation at the DRI LTC/SNF Seminar].
- Centers for Medicare & Medicaid Services. (2015). State Operations Manual – Appendix PP – Guidance to Surveyors for Long-term Care Facilities. Retrieved 02/23/16.
- Compliance Solutions for the Perfect Survey Every Day. (2014). F322. Retrieved 02/23/16 from The Perfect Survey website.
The Power of a Nurse’s Words
Wednesday, March 23rd, 2016
We here at ALN sometimes encounter a sense of “Am I making a difference and is it enough?” in our profession. And it’s interesting to hear that same thing from other nurses. Diane M Goodman recently posted a piece that so compelled us, we just had to share. Thank you, Diane.”
Sticks and Stones; The Power of a Nurse’s Words
By Diane M. Goodman, Originally appeared in MedScape, Jan 21, 2016
Many of us were raised in a generation by mothers who warned us of the old English adage about taunting others through the use of name-calling and words. We knew better. Words could either be unbelievably comforting or leave lasting scars on our memories.
As nurses, our words and our voices are no less profound. We can change the trajectory of a life by coaxing change from a desultory or despondent patient, and we can inspire peers to greatness when they feel they cannot work another moment or another busy day.
Sharing research with peers may allow them to comprehend the improbability of what we DO on a daily basis. By reading a quantitative time-study, for example, and sharing it with colleagues, they may have an improved understanding of why nurses need stress management techniques to perform their jobs. Nursing is extremely difficult work. Expecting substantive conversation or specific phrases to “just happen” at the bedside is like asking the typical pilot to land an airplane on the Hudson!
Nurses, on the average, complete >70 (!!) tasks per hour. Nurses change tasks approximately every 55 seconds. They are also interrupted approximately once every 32 minutes, with the highest amount of interruptions recorded during medication administration!*
Why is it important to know this? While this time/event study was conducted in Sydney, the research was rigorous enough to be utilized internationally as an example of why nurses may find it “difficult” to bond with patients. We may be groping to find the right words to instill initiative, hope, and change in our patients. We could even be struggling a bit.
Nina (not her real name) reminded me of this in ICU. I was struggling. She was paralyzed, intubated, ventilated, and so, so sick. I was sure she would not survive. She was only 19.
I was exhausted every night, hanging more blood, platelets and medications than I had ever hung in my life. She was septic and she had leukemia. “Sticks and stones”, I repeated in my head over and over, warning myself not to frown or sigh, or show tiredness EVER. Instead, I stroked her hair, and told her how much I loved my little sister, and my dogs. I played music for her when my voice got tired or I ran out of words. If nothing sweet or positive was left to be said, I smiled and hummed, night after exhausting night. OK, so I did a lot of humming.
Her bed was empty one night, as ICU beds often are. Rehab, they said. Long-term. Newer, sicker patients came and went.
Six months later, a young, attractive woman was wheeled in with a huge family circling her, including one very determined sister. It was Nina. She remembered nothing of her stay but a woman who stroked her hair and hummed and talked softly of dogs and family. I would have given her almost zero odds of surviving, and here she was!! Sitting tall, with very little residual effects. I couldn’t believe she remembered me! She remembered nothing else.
CMS Interpretive Guidelines – Revisions to Restraints Guidance
Monday, January 25th, 2016
As part of ALN Consulting’s commitment to our legal partners, we introduce the second installment of our CMS Interpretive Guidelines series by diving into the revisions on the use of restraints. The guidelines include an explanation of the intent of the law, definitions of terms, and instruction on determining compliance with the law. The most important update to the Interpretive Guidelines regarding restraints prohibits their use in fall prevention. This update significantly impacts the defense of long term care facilities. These revisions must be studied thoroughly in order to build a firm case for the use or non-use of restraints. Continue reading for a thorough explanation of these revisions in the Interpretive Guidelines.
42 C.F.R. §483.13(a).
The CFR Regulation states, “The resident has the right to be free from any physical or chemical restraints imposed for purposes of discipline or convenience, and not required to treat the resident’s medical symptoms.” Relevant definitions in the Interpretive Guideline include:
Chemical Restraint: any drug that is used for discipline or convenience and not required to treat medical symptoms.
Convenience: any action taken by the facility to control a resident’s behavior or manage a resident’s behavior with a lesser amount of effort by the facility and not in the resident’s best interest.
Discipline: any action taken by the facility for the purpose of punishing or penalizing residents.
Freedom of movement: any change in place or position for the body or any part of the body that the person is physically able to control.
Medical Symptom: an indication or characteristic of a physical or psychological condition.
Physical Restraints: any manual method or physical or mechanical device, material, or equipment attached or adjacent to the resident’s body that the individual cannot remove easily which restricts freedom of movement or normal access to one’s body.
Removes easily: means that the manual method, device, material, or equipment can be removed intentionally by the resident in the same manner as it was applied by the staff (e.g., side rails are put down, not climbed over) considering the resident’s physical condition and ability to accomplish objective (e.g., transfer to a chair, get to the bathroom in time).
Regulation Tag F222 Guidance on Restraints
The main principal in the Interpretive Guideline is that restraints may not be used for staff convenience, and the only acceptable use of a restraint is to treat a medical symptom, with a physician order. The order itself is not justification to use a restraint, but must be “viewed in the context of the resident’s condition, circumstances, and environment.” In addition, as a measure of last resort restraints can be used to protect the safety of the resident or others for a brief period of time. The facility may not use restraints in violation of the regulation solely based on a legal surrogate or representative’s request or approval.
When a restraint has been used, the surveyor must determine if the facility followed a systematic process of evaluation and care planning prior to using restraints, and if the plan of care was consistently implemented.
Surveyor “Probes” in facility use of Restraints
The defense team can use the “probes” or questions posed by the Interpretive Guidelines for surveyors in cases which involve restraints:
- What are the medical symptoms that led to the consideration of the use of restraints?
- Are these symptoms caused by failure to:
- Meet individual needs in accordance with the resident assessments
- Use rehabilitative/restorative care?
- Provide meaningful activities?
- Manipulate the resident’s environment, including seating?
- Can the causes of medical symptoms be eliminated or reduced?
- If the causes cannot be eliminated or reduced, then has the facility attempted to use any alternatives in order to avoid a decline in physical functioning associated with the restraint use?
- If alternatives have been tried and deemed unsuccessful, does the facility use the least restrictive restraint for the least amount of time? Does the facility monitor and adjust care to reduce the potential for negative outcomes while continually trying to find and use less restrictive alternatives?
- Did the resident or legal surrogate make an informed choice about the use of restraints? Were the risks, benefits, and alternatives explained?
- Does the facility use the CAA’s to evaluate the appropriateness of restraint use?
- Has the facility reevaluated the need for the restraint, made efforts to eliminate its use and maintained residents’ strength and mobility?
Updates to the Interpretive Guidelines
The most recent update to the Interpretive Guidelines for restraints was published in November 2014. The examples of facility practices that met the definition of restraint was noted to be “not limited to” the list. Also, in discussion of side rails, the addition of “assist with physical functioning” was added as an acceptable use.
The most important update to the Interpretive Guideline stated, “Falls do not constitute self-injurious behavior or a medical symptom that warrants the use of a physical restraint. Although restraints have been traditionally used as a falls prevention approach, they have major, serious drawbacks and can contribute to serious injuries. There is no evidence that the use of physical restraints, including but not limited to side rails, will prevent or reduce falls. Additionally, falls that occur while a person is physically restrained often result in more severe injuries (e.g., strangulation, entrapment).”
This update has implications in the defense both of the use or non-use of restraints, as well as in matters involving falls. When understood and implemented, these interpretive guidelines can be crucial in the defense of long term care facilities.
In conclusion, the successful defense of long term care facilities relies on a thorough understanding of the CMS Interpretive Guidelines. With our expertise, ALN Consulting can advise your legal team on how to best navigate the complicated CMS Interpretive Guidelines to support your legal team’s defense. Let us help you decipher the latest revisions of the Interpretive Guidelines and strengthen your long term care case.
References
- Harris, Rick E. (2015). How to Use the CMS Surveyor Guidance to Craft a Winning Defense [Presentation at the DRI LTC/SNF Seminar].
- Centers for Medicare & Medicaid Services. (2015). State Operations Manual – Appendix PP – Guidance to Surveyors for Long Term Care Facilities. Retrieved 01/04/16.
Understanding The Four Elements of Negligence
Thursday, December 3rd, 2015
Understanding the four elements of negligence are essential to evaluating a malpractice case. Since early American law was formed, negligence was considered a distinct tort in which a person was held subject to liability for carelessly causing harm to another. In order to prove negligence, a plaintiff is required to show each of the following:
- The defendant owed the plaintiff a specific duty.
- The defendant breached this duty.
- The plaintiff was harmed.
- The breach of duty caused the harm.
Some legal scholars also hold forth a fifth essential element: proximate cause, which is considered under the umbrella of the causation in the fourth element.
Negligence vs. Malpractice
The Joint Commission defines negligence as “failure to use such care as a reasonably prudent and careful person would use under similar circumstances.” Malpractice is defined as “improper or unethical conduct or unreasonable lack of skill by a holder of a professional or official position; often applied to physicians, dentists, lawyers, and public officers to denote negligent or unskillful performance of duties when professional skills are obligatory. Malpractice is a cause of action for which damages are allowed.”
Negligence is an unintentional tort, and the four elements above must be present. Malpractice goes one step further and refers to a tort committed by a professional acting in his or her professional capacity.
Professional Negligence
When a nurse or doctor is sued for malpractice, they are accused of negligence which harmed an individual in the course of his or her role as a medical professional. Defined in a nursing malpractice situation by the Black’s Law Dictionary, professional negligence is “the doing of something which a reasonably prudent person would not do, or the failure to do something which a reasonably prudent person would do, under circumstances similar to those shown by the evidence. It is the failure to use ordinary or reasonable care.”
Nursing Malpractice
The NSO, which is the largest professional liability insurance provider for nurses, has examples of nursing malpractice legal case studies and subsequent verdicts for review. They range from a Foley catheter used incorrectly which caused a urethral tear, to failure to prevent decubitus ulcers. If you are interested in reading the case studies in full, click on the following links:
http://www.nso.com/risk-education/individuals/legal-case-study/Nurse-Catheterization-for-life
References
- Stubenrauch, James M. (2007). Malpractice vs. Negligence. AJN, American Journal of Nursing, 107(7), 63-63. Retrieved from Lippincott Nursing Center database: http://www.nursingcenter.com/journalarticle?Article_ID=727909
- Owen, David G. (2007) “The Five Elements of Negligence,” Hofstra Law Review: Vol. 35: Iss. 4, Article 1. Available at: http://scholarlycommons.law.hofstra.edu/hlr/vol35/iss4/1
- Ashley, Ruth C. (2003). Understanding Negligence. Critical Care Nurse, 23(5), 72-73. Retrieved from Critical Care Nurse database: http://ccn.aacnjournals.org/content/23/5/72.full
- (2015). Legal Case Studies. Retrieved October 8, 2015, from NSO website: http://www.nso.com/risk-education/individuals/legal-case-study/Nurse-Catheterization-for-lifehttp://www.nso.com/risk-education/individuals/legal-case-study/Nurse-Decubitus-ulcer-improperly-treated
- Black HC. Black’s Law Dictionary. 9th ed. St. Paul, Minn: West Publishing Company; 1998.
