Archive for the ‘MedMal’ Category
The Law and the Glasgow Coma Scale
Monday, November 7th, 2016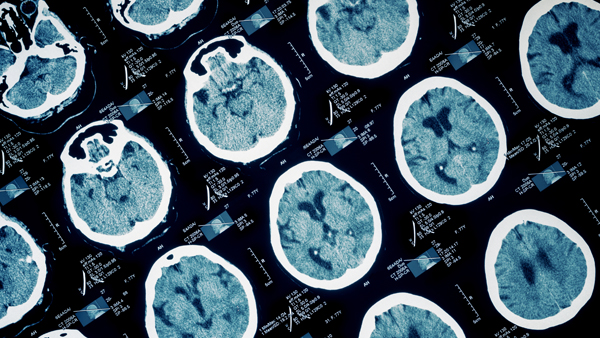
When pursuing legal action for clients who have sustained a traumatic brain injury (TBI), attorneys must be able to assess the progression of damage and the prognosis for recovery. One of the first steps is understanding the most common scoring system used to describe and record levels of consciousness in persons with an acute brain injury. Known as the Glasgow Coma Scale (GCS), the scale is a practical method of assessing impaired conscious level in persons injured from any cause, although it is most frequently used in cases of head injury.
First described in 1974 by neurosurgeons at the University of Glasgow, Scotland, the GCS was developed to provide a “universal” method of describing the responsiveness of a patient in simple, objective terms. The verbiage has evolved since its introduction, but the scale itself has largely remained the same over time. It has become a critical tool for first responders, paramedics, and emergency room staff for measuring the degree of an acute brain injury.
The GCS measures functions involving eye opening, verbal response, and motor response. On a scale ranging between 3 and 15, a score below 8 indicates a severe injury, while 13 and above is considered a mild impairment. Clinicians use this scale to rate the best eye opening response, the best verbal response, and the best motor response an individual makes. The final GCS score is the sum of the number points in those categories. A modified version of the GCS is the Pediatric Glasgow Coma Scale (PGCS) which considers the eye, verbal, and motor response tests separately as well together.
This scoring system guides initial medical decisions and monitors changes in responsiveness. It is useful in monitoring chronic patients in intensive care. But even out of the ICU, the scale helps nurses spot important changes in a patient’s condition. The timing and frequency of the assessment is individualized. The role of the scale is to support and not replace clinical decision making.
Measuring Traumatic Brain Injury Response
The adult Glasgow Coma Scale measures functions as follows:
Eye Opening (E)
- 4 – Spontaneous
- 3 – In response to voice
- 2 – In response to pain
- 1 – None
Verbal Response (V)
- 5 – Normal conversation
- 4 – Disoriented conversation
- 3 – Incoherent words
- 2 – No words, only sounds
- 1 – None
Motor Response (M)
- 6 – Normal
- 5 – Localized to pain
- 4 – Withdraws to pain
- 3 – Decorticate posture (an abnormal posture that can include rigidity, clenched fists, legs held straight out, and arms bent inward toward the body with the wrists and fingers bend and held on the chest)
- 2 – Decerebrate posture (an abnormal posture which can include rigidity, arms and legs held straight out, toes pointing downward, head and neck arched backwards)
- 1 – None
The Glasgow Coma Scale is not without its limitations. It only indicates a conscious level at the time the test is administered. By itself, it does not reveal how long someone has been unconscious or even, in the case of a high score, that he or she was unconscious at all at a previous point. A dead patient can still be assigned a GCS of 3.
Some researchers are concerned with the GCS’s poor inter-rater reliability, or degree of agreement or consensus among those assessing a patient’s condition. It can also limited by the training a first responder or paramedic has in identifying and assessing brain injury.
A measurable level of brain injury can fluctuate significantly over minutes or hours – especially considering factors like shock, low blood oxygen, and the presence of drugs or alcohol in a patient’s system. A GCS score can obviously improve by the time the patient reaches the emergency room. A very low score does not mean that a patient will never recover from his or her TBI. Likewise, a very high score does not mean that there is no brain injury present. The Glasgow Coma Scale complements, rather than substitutes, other neurological assessments.
When an accident involves a traumatic brain injury, time can be as valuable a resource as money for plaintiffs, defendants, and attorneys alike. Explicating all the fine points of consciousness and TBI takes plenty of both. A legal nurse consultant reviews client medical records and independently investigates the case. Your LNC can help your legal team determine a case’s merit and efficiently pinpoint medical issues and other factors that will affect how you proceed.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.
Kennedy Terminal Ulcer – A 2016 Update
Sunday, October 23rd, 2016
2016
In April 2016, the National Pressure Ulcer Advisory Panel or NPUAP announced a change in the terminology and the stages of pressure injuries. Though these stages continue to include both unstageable pressure injuries and deep tissue pressure injuries the new definitions do not specifically mention the Kennedy Terminal Ulcer. Over the years, however, multiple panels and advisory groups have documented the Kennedy Ulcer as an end of life phenomenon.
The unavoidable skin breakdown that occurs as part of the dying process, known as a Kennedy Ulcer, has been recognized by Ostomy Wound Management since a 2009 journal article. Also in 2009, an expert panel released a consensus statement known as SCALE or Skin Changes At Life’s End which identified skin organ compromise occurring at the end of life. The panel recognized that the ulcer is usually seen on the coccyx or sacrum but has been reported in other anatomical areas and is usually associated with imminent death.
This special classification was also mentioned by the Center for Medicare and Medicaid Services (CMS) in 2014 within its Quality Reporting Program Manual and its Continuity Assessment Record and Evaluations Data Set (CARE) for long-term care hospitals. The “Coding Tips” of the publication noted if an ulcer was part of the dying process, developing from six weeks to two to three days before death, it should not be coded as a pressure ulcer.
Click here for the full detailed staging guidelines.
ALN Consulting will continue to stay on top of these and other developments. Contact ALN Consulting if you have questions about a case and would like an initial consultation.
2015
This portion originally published on October 26, 2015:
It is well known that a pressure ulcer is an area of skin that breaks down when pressure on the skin reduces blood flow to the area. However, the knowledge and acceptance of skin failure at the end of life from various etiologies, including the Kennedy Terminal Ulcer (KTU), is growing among evidence based practitioners. The Kennedy Terminal Ulcer and other unavoidable similar skin phenomenon such as Skin Failure, SCALE (Skin Changes at Life’s End), Deep Tissue Injury (DTI), and the Tremblay-Brennan Terminal Tissue Injury were addressed at the most recent VCU Pressure Ulcer Summit by experts and scholars in the field.
The Kennedy Terminal Ulcer was first described by Karen Lou Kennedy in 1989, and evidence of poor perfusion to the skin causing a pressure ulcer-like damage of soft tissue in serious illness and at the end of life is well documented. While there are several etiologies that could cause unavoidable skin failure, the Kennedy Terminal Ulcer is focused on soft tissue injury on bony prominences, usually on the sacrum, during the dying process.
As illustrated in the photos, the Kennedy Terminal Ulcer has a sudden onset of a purple/red blister or abrasion, and rapidly progresses to a Stage III or IV ulcer. While further research is required, and was recommended by the PU Summit, there is general consensus that if a dying patient has blood perfusion issues that affect many other organs, known as multi-organ failure, then it is reasonable to accept that the lack of blood perfusion also can affect the skin resulting in unavoidable soft tissue injuries, despite adequate prevention measures.

Kennedy Terminal Ulcer

A phenomenon called “3:30 Syndrome” presented as a subdivision of the Kennedy Terminal Ulcer, which forms more quickly and appears as black spots.
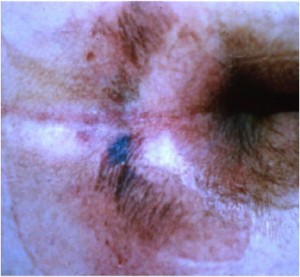
The classic “butterfly” or “horseshoe” shape of the Kennedy Terminal Ulcer.
In the near future the ANCC Magnet commissioners plan to develop and create access to a Magnet Designated Facility Database for hospital acquired pressure ulcers (HAPU) to promote ongoing research for unavoidable pressure ulcers and uncharacteristic soft tissue injuries that occur despite appropriate implementation and escalation of interventions to prevent skin injury and ulcers at the end of life.
References
- Brindle, Creehan, Black, & Zimmerman. (2015). The VCU Pressure Ulcer Summit: Collaboration to Operationalize Hospital-Acquired Pressure Ulcer Prevention Best Practice Recommendations. J Wound Ostomy Continence Nursing, 2015:00(0):1-7.
- Kennedy-Evans, Karen. (2012). The Life and Death of the Skin. [Nursing Home/ALF Litigation Seminar].
- Kennedy Terminal Ulcer. (2014). Retrieved October 7, 2015, from Kennedy Terminal Ulcer web site: http://www.kennedyterminalulcer.com/
Measuring Pain and Suffering
Monday, October 17th, 2016
It doesn’t take an attorney to know that pain and suffering go beyond an initial physical injury. Mental pain and suffering often ranges from lack of sleep or energy to humiliation, hypervigilance, consuming anger, mood swings, sexual dysfunction, and even PTSD (Post-Traumatic Stress Disorder). In a nutshell, an accident or injury can impact someone’s enjoyment of life. Plaintiff attorneys must quantify not only the physical and mental pain and discomfort a client has already experienced, but also what an expert can reasonably predict in the future.
A comparatively minor accident has far-reaching ramifications of which a judge or jury may not conceive. A pedestrian with the right-of-way can be hit in the crosswalk by a car, but ultimately walk out of an emergency room without broken bones or significant physical trauma. But a diagnosis of soft tissue damage doesn’t spell out that the person has been unable to sit without pain for a year. It doesn’t convey that he or she experienced nightmares for weeks, feared crossing streets for months, or was unproductive due to physical pain and an erratic sleeping pattern.
Even if a victim’s livelihood doesn’t involve significant physical labor, pain and discomfort find their way into a daily work life. Moving around with pain in what seems like an undemanding job can slow a person down. A part-time administrative professional can be laid off for cutting hours back to attend physical therapy…and be forced to hunt for a new job in between doctor’s appointments and pain that doesn’t follow a schedule.
For that hypothetical pedestrian, consequences like these were caused by the defendant. That pedestrian is entitled to compensation for all of the consequences – particularly, the mental or financial effects that remain long after the bones have healed and the bruises have disappeared. The law even recognizes mental pain and suffering of a less catastrophic nature – such as being unhappy about missing a family wedding because of post-incident physical limitations or pain. But the less obvious the effects, the greater the onus on the plaintiff to prove that the amount of damages sought are reasonable.
There are palpable odds stacked against anyone who seeks legal relief for pain and suffering. Negligence claims require a solid establishment of causation between the defendant’s actions and the negative effects on a plaintiff’s life. Plaintiff attorneys should establish that the client took reasonable steps to minimize or mitigate damages done, including seeking medical attention in a timely manner. Compensation can be reduced if he or she can even be considered partially responsible for an accident. Even a legitimate delay in diagnosis or treatment can hurt a case.
Along with the letter of the law, plaintiffs are up against juries with limited, subjective knowledge. In general, juries are not offered concrete guidelines for quantifying the value of pain and suffering. Mostly they use their common sense and personal background – which is highly variable and colored by personal opinions.
And like members of a jury, plaintiffs come out of the general population. A witness with limited communication skills may not be able to fully and accurately convey the mental or physical effects. It is also challenging to measure the pain and suffering of an accident victim who is not alive to testify on his or her own behalf. A plaintiff’s likeability and credibility can sway jury opinions.
The litigious society we live in makes it all the more important for a professional with a specific skill set to review and explain the physical and mental repercussions of an incident. Plaintiffs need as much solid evidence as possible to counteract a jury’s skepticism. And yet an endless string of witnesses and extensive medical records can overwhelm and confuse a jury more than edify them.
Documenting Pain And Suffering
That’s why it behooves a plaintiff to request a separate pain and suffering report. Also known as a FRE 1006 summary witness report, this is a special request that can be completed by a legal nurse consultant (LNC). Evaluating non-economic, non-concrete damages takes special expertise that someone with both legal and medical acumen can offer. An LNC can review complex, extensive medical records and summarize pain and suffering in ways that laypeople in a jury box can relate.
On one hand, this report humanizes the suffering victim in a way that a diagnosis can’t translate. On the other hand, a clearly detailed report in clinical terms can document how the subject’s life has changed as a result of someone else’s mistake.
At the end of the day, in fact, pain and suffering is often a repercussion of someone else’s poor decisions. By treating it with the same consideration as high blood pressure, for example, a plaintiff’s legal team can move closer to achieving a fair and reasonable settlement for a client.
Strengthen your case with a FRE 1006 summary witness report from ALN Consulting.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.
National Pressure Ulcer Advisory Panel (NPUAP) Release New Clinical Guidelines and Taxonomy for Pressure Injuries
Friday, October 7th, 2016
In 1986, the National Pressure Ulcer Advisory Panel (NPUAP) was formed as an independent, non-profit organization established to ensure consistent prevention, management and research of pressure ulcers. Conflicts in research and prevention created the need for this governing body, an organization that would work to create guidelines and establish best practices surrounding pressure injury wounds. NPUAP serves as the authoritative voice for improved patient outcomes in pressure ulcer prevention and treatment through the development of public policy, education and research.
Subsequent to the formation of NPUAP, the terminology to describe “pressure ulcers” was redefined and the staging system of pressure wounds expanded. Although changes were made with the intent of clarifying the differences among the stages of pressure ulcers, the new classification system led to more confusion. For example, the use of the term “injury” and “ulcer” interchangeably caused great confusion.
In April 2016, a consensus conference was convened by NPUAP to review and revise the pressure injury staging system and to standardize the terminology used to describe injury to the skin from external pressure. The term “pressure ulcer” was changed to “pressure injury.” This simple change in terminology was actually monumental, as it was a major departure from the old taxonomy in the 30 years since the panel was formed. Updates to the panel’s description of the stages of pressure injuries were developed. The group indicated that the change in terminology would more accurately describe pressure injuries to both intact and ulcerated skin.
The 2016 definition of “Pressure injury” by NPUAP describes localized damage to the skin and underlying soft tissue usually over a bony prominence, related to a medical procedure such as prolonged surgery or from a medical device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shearing forces. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue. Shearing occurs from friction against the skin that leads to a superficial or partial thickness injury, often resembling an abrasion.
Pressure Injury Staging
The staging system further defined pressure injuries of stages 1-4 as well as including medical device related pressure injuries and mucosal membrane pressure injuries. The following illustrations denote each stage and classification of pressure injuries.
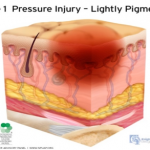 Stage 1 Pressure Injury: Non-blanchable erythema of intact skin. Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple of maroon discoloration; these may indicate deep pressure injury.
Stage 1 Pressure Injury: Non-blanchable erythema of intact skin. Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple of maroon discoloration; these may indicate deep pressure injury.
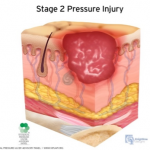 Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible nor are deeper tissues. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible nor are deeper tissues. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
Stage 3 Pressure Injury: Full-thickness skin loss. Full thickness loss of skin, in which adipose tissue is visible in the ulcer, meets the definition of a Stage 3 pressure injury. Granulation tissue and epibole (rolled wound edges) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss, this becomes an Unstageable Pressure Injury.
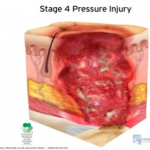 Stage 4 Pressure Injury: Full-thickness skin and tissue loss. Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole, undermining and/or tunneling often occur. The depth of the injury varies by anatomical location. If slough or eschar obscures the extent of tissue loss, an injury such as this would be described as an Unstageable Pressure Injury.
Stage 4 Pressure Injury: Full-thickness skin and tissue loss. Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole, undermining and/or tunneling often occur. The depth of the injury varies by anatomical location. If slough or eschar obscures the extent of tissue loss, an injury such as this would be described as an Unstageable Pressure Injury.
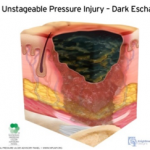
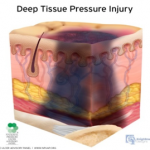 Deep Tissue Pressure Injury: persistent non-blanchable deep red, maroon or purple discoloration. This type of injury may involve either intact or non-intact skin, presenting with a localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss.
Deep Tissue Pressure Injury: persistent non-blanchable deep red, maroon or purple discoloration. This type of injury may involve either intact or non-intact skin, presenting with a localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss.
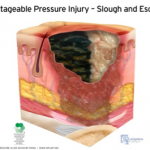
 Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss. This type of injury involves full-thickness skin and tissue loss. The extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If the slough or eschar is removed from the wound, a stage 3 or stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss. This type of injury involves full-thickness skin and tissue loss. The extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If the slough or eschar is removed from the wound, a stage 3 or stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
As classifications and guidelines change, it’s critical to have an expert on your team who understands the current definitions. ALN Consulting’s team of legal nurse consultants have their finger on the pulse of these changes, and are trained to spot inaccuracies in medical records that can effect case outcomes. Contact ALN Consulting today to learn how we can help.
ALN Litigation Perspective
Monday, October 3rd, 2016
Fudge & McArthur, P.A.’s Donna Fudge and Benjamin Broadwater announce victory in recent Stage IV Pressure Ulcer/Nursing Home case in Florida.
The complexity of circumstances demonstrated in this case is not atypical of the facts in many of the long-term care cases in litigation today. The importance of cohesion between the medical and legal defense teams cannot be emphasized enough in these cases. From both a clinical and legal standpoint, considerable skills are required to weed through the minutia of what was likely an abundance of medical records and break down the case facts simply into a bad outcome despite the rendering of good care. Of significance in this case was the team’s ability to use the medical record to create the picture of collaborative care provided in the absence of wound documentation. Unfortunately, all too often we see key portions of the medical record are missing, requiring our nurse consultants to hunt for the pieces of the puzzle necessary to reconstruct the plan of care and develop a fail-safe defense strategy.
Defense Jury Verdict: Morgan & Morgan, P.A. represented the Estate of Willie F. Coley, in a lawsuit against TR & SNF, Inc., d/b/a The Nursing Center at University Village, and BVM Management, Inc. in relation to Mr. Coley’s 12+ year residency at University Village’s skilled nursing facility. The Complaint alleged negligence for the development of a Stage IV sacral/coccyx pressure ulcer. Mr. Coley passed away 15 months after leaving University Village and continued to have this pressure ulcer until the time of his death. A graphic photograph of the Stage IV ulcer was shown to the Jury.
This case focused on the final three months of Mr. Coley’s 12+ year residency at University Village. Plaintiff alleged that University Village failed to implement appropriate interventions after re-admission from a hospital stay, and failed to revise any interventions after Mr. Coley developed his sacral/coccyx ulcer, in violation of the Federal Regulation for pressure ulcers, FTag 314. Plaintiff also alleged that the caregivers failed to follow the Facility’s own Policies and Procedures by failing to monitor/track the wound, and by failing to provide adequate pressure relief every 2 hours. As a result, Plaintiff alleged that University Village failed to prevent the development, and worsening, of Mr. Coley’s pressure ulcer. Lastly, Plaintiff alleged that the University Village caregivers failed to properly assess and treat Mr. Coley for Pain allegedly associated with his wound
Defense Themes: The defense focused on Mr. Coley’s 10 most recent Hospitalizations leading up to his coccyx skin wound and his 20 underlying Comorbidities including a history of cerebrovascular accident, stercoral ulcer, dementia, paralysis, C. difficile, and GERD which contributed to Mr. Coley’s development and eventual worsening of his sacral/coccyx ulcer. The Defense proved that proper interventions were put in place when Mr. Coley was re-admitted from the hospital, but despite these interventions, Mr. Coley experienced an unavoidable “Friction Blister” that progressed to a pressure ulcer and eventually became a Stage IV with suspected osteomyelitis. The jury heard expert testimony that the healing of Mr. Coley’s left and right Buttocks skin wounds, adjacent to his Coccyx sore, was evidence that he was being properly offloaded in that area. The Defense argued that it met FTag 314 by: (1) evaluating Mr. Coley’s risk factors for additional pressure sores, (2) implementing interventions for the prevention of pressure sores, (3) monitoring the impact of those interventions by notifying the physicians of changes in the wound and obtaining new treatment orders such as a wound vac and an infectious disease consult, and (4) revising those interventions.
Overcoming Documentation Problems: The nursing home had lost its wound tracking documentation. However, the Defense argued that any lack of documentation did not mean that there was a lack of monitoring. The staff consistently notified Mr. Coley’s physicians of changes in the wound’s condition, and a wound care physician was tracking the wound on a weekly basis from April 23, 2014 through June 4, 2014. The Defense pointed out to the jury that Plaintiff’s allegations were based on records that were “cherry picked” and it was explained that, in order to get a true and accurate understanding of the interventions such as re-positioning, pain management and wound monitoring by the caregivers, the jury had to look at the entirety of Mr. Coley’s Chart, which was filled with evidence that these areas of care were actually provided.
Jury Verdict: Following the 5 day jury trial, the jury returned a defense jury verdict in favor of both Defendants.
Trial Team: Donna Fudge and W. Benjamin Broadwater of Fudge & McArthur, P.A. were lead trial counsel. Caitlin Kramer, Esq., and Paralegals Amy Bozarth and Julie Christ of Fudge & McArthur, P.A. assisted in the trial.
Defense Experts: Dr. Aimee Garcia (Houston, Texas) and Alexa Parker Clark (St. Petersburg, Florida)
It’s the complex cases such as this one which demonstrate the essential need for synergy between the medical and legal defense teams. ALN Consulting’s team of experts are trained to quickly identify key pieces of evidence that are missing or have been falsified. We can piece together a solid picture from numerous records, giving legal teams a clear path to case resolution.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.
Medicinal Marijuana Linking to Decline in Overdoses
Friday, August 19th, 2016
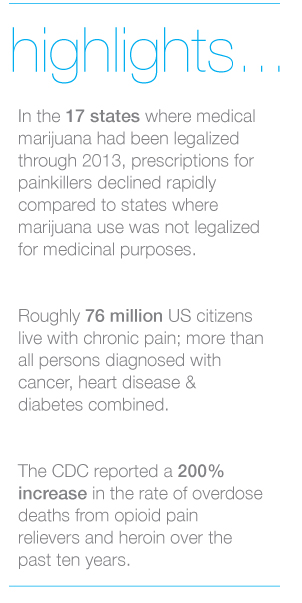
The Washington Post reports that University of Georgia researchers have produced significant evidence linking prescription marijuana to falling overdose statistics in states where medicinal marijuana use is legal.
The study suggests that chronic pain sufferers can find alternatives to dangerous medication on a large scale. While this development hasn’t come without push back from pharmaceutical lobbyists, states that have legalized medical marijuana have already seen a plunge in painkiller prescriptions.
The Georgia researchers reported that in the 17 states where medical marijuana use had been legalized through 2013, prescriptions for painkillers and other classes of medications declined rapidly compared to states where marijuana use was not legalized for medicinal purposes. The number of prescriptions for medications commonly used to treat chronic pain, such as antidepressants, anti-nausea, anti-anxiety and seizure medications decreased across the board. However, the most striking finding was the consistent drop in prescriptions written for analgesics or painkillers.
 The study conducted by the University of Georgia researchers adds more information to the rapidly growing pool of knowledge supporting marijuana use for treatment of chronic pain, both in combination with opioids and as a viable treatment on its own.
The study conducted by the University of Georgia researchers adds more information to the rapidly growing pool of knowledge supporting marijuana use for treatment of chronic pain, both in combination with opioids and as a viable treatment on its own.
Chronic pain is common, multidimensional and individualized and treatment can be challenging for healthcare providers as well as patients. Roughly 76 million US citizens live with chronic pain; a number larger than all persons diagnosed with cancer, heart disease and diabetes combined.
In March of this year, the Centers for Disease Control and Prevention (CDC) updated guidelines for clinicians who prescribe opioids for individuals suffering from chronic pain.
The guidelines help providers make informed decisions about pain treatment for patients 18 and older in primary care settings. The CDC recommendations focus on the use of opioids in treating chronic pain and are not intended for patients actively being treated for cancer and those receiving palliative or end-of-life care.
Unlike cannabis, opioids carry a known risk of chemical dependence. Over ten years ago, the CDC reported a 200% increase in the rate of overdose deaths from opioid pain relievers and heroin.
This finding has several implications for the investigation of medical malpractice cases. Where cannabis is not legally available, patients may increasingly seek it on the black market and complicate a medical investigation. The full ramifications of medically prescribed cannabis may not be known for many years, and with decreasing revenue at stake, the pharmaceutical industry continues to fund studies discounting its benefits. Most immediately, the role of prescription drugs in a case is affected by the state in which an adverse medical event took place. Finding expert witnesses conversant in drug laws of that state will be more important than ever.
ALN Consulting can research, identify and secure expert witnesses appropriate for cases involving the use of medical marijuana and other pain treatments. We do more than help you prepare…we prepare you to win, call us today.
Uncovering False Allegations
Wednesday, August 3rd, 2016
ALN was presented with a long term care case with allegations related to respiratory failure and death. At the time of the events in question, the plaintiff, Ms. Maggie White, was an 84-year-old female with a past medical history of coronary artery disease, chronic obstructive pulmonary disease, hypertension, anxiety, Alzheimer disease, chronic low back pain and lumbar disc degeneration. Ms. White was admitted to the defendant facility, a skilled nursing center, for rehabilitation after receiving epidural steroid injections for chronic low back pain.
Upon admission, care was implemented to include physical therapy and occupational therapy. During the course of residency, Ms. White developed a cough which progressed to chest congestion with decreased breath sounds. Prescribed treatment included cough suppressants, antibiotics, nebulizer treatments, and steroids. Ms. White’s chest x-ray was clear; her respiratory symptoms improved with treatment, but subsequently developed edema of the lower extremities bilaterally. Lasix was prescribed which resolved the extremity edema. Three days later, Ms. White was again found to have diminished breath sounds and labored respirations requiring a hospital admission. Admitting diagnoses included congestive heart failure (CHF) and cardiomegaly with respiratory failure. Ms. White was intubated and placed on ventilator support. Despite multiple consultations and treatments, Ms. White’s CHF worsened and she expired three days later.
Plaintiff’s counsel alleged that the defendant facility failed to properly assess Ms. White’s respiratory status and failed to provide timely treatment for shortness of breath, alleging the symptoms existed for days prior to transfer. Plaintiff’s counsel further alleged her respiratory failure and death were caused by the defendant facility’s negligence.
False Allegations Identified With Legal Nurse Review
Upon review of the facility records, ALN’s nurse reviewer was able to refute allegations of inappropriate assessment, as well as the existence of respiratory distress in the days prior to transfer. The investigation confirmed that the facility staff properly assessed, reported, and monitored Ms. White’s clinical status per facility protocol and long-term care guidelines. Although it was believed this information was enough to present an adequate defense, the ALN nurse reviewer dug deeper into the hospital records, striving to ensure the best possible defense was developed for the client.
Further investigation into Ms. White’s condition and circumstances surrounding her death revealed a myriad of possible contributing/causative factors. Ms. White had a recent diagnosis of possible heparin-induced thrombocytopenia (HIT). Research revealed that the most common complication of HIT is venous thromboembolism, including pulmonary embolism. Subsequent to Ms. White’s hospital transfer, the nurse reviewer’s investigation revealed that the physician consultants had conflicting opinions related to the cause of Ms. White’s respiratory deterioration. One theory the consultant considered was that Ms. White’s respiratory deterioration was possibly caused by a pulmonary embolism. In spite of this, Ms. White was never evaluated or treated for a pulmonary embolism or HIT. Although the resident was admitted with CHF, Ms. White was never adequately treated for the condition. Diuretics, a staple in CHF treatment, were discontinued – quite possibly contributing significantly to Ms. White’s declining heart function. Of further consideration was the fact that records indicated Ms. White had a probable new diagnosis of lymphocytic leukemia, which was never fully evaluated or treated. Investigation into Ms. White’s history revealed previous chest x-rays with evidence of pulmonary nodules which were never evaluated or treated. The cause of Ms. White’s death was listed as respiratory failure. As the ALN reviewer determined, the etiology of the resident’s respiratory failure was never confirmed and could have been the result of any number of conditions diagnosed after her rehabilitation stay at the defendant facility, which were not adequately evaluated or treated.
On initial review of the defendant facility records, the ALN reviewer was able to produce evidence showing the facility met the standard of care for evaluation and treatment of the respiratory symptoms Ms. White developed while a resident at the Defendant facility. The ALN reviewer’s in-depth investigation into Ms. White’s comorbid conditions and history revealed a myriad of possible sources for Ms. White’s respiratory failure and death – greatly expanding the client’s ability to argue against the facility’s liability and help mitigate possible damages.
In this case, the expertise of the ALN nurse reviewer was crucial in identifying possible contributing factors and raising questions regarding causation and mitigating factors – factors which would have gone unnoticed by a non-clinical professional. ALN Consulting’s team of nurse consultants are in a unique position to build the strongest, most manageable court case for their clients. We find the root issue by digging deeper.
ALN Consulting is a national provider of medical-legal consulting services, founded in 2002. Our expertise includes, yet is not limited to, medical malpractice, long-term care, product liability, class action/mass litigation, and toxic tort. Contact Us to put our legal nurse consulting experts on your case.
Culpability and Electronic Health Records (EHRs)
Tuesday, June 14th, 2016
Using Electronic Health Records (EHRs) can be an excellent way for medical professionals and their staff members to care of patients more easily, sending and receiving information when seconds matter in making medical decisions. However, there are also some serious considerations with EHRs, and one of those main considerations is culpability. Specifically, the question becomes who is culpable when something goes wrong. Is the onus on the medical staff to catch mistakes, or is it on the EHR system and the company that designs and manages that system to catch mistakes before they reach the medical staff?
The EHRs and the Companies That Create Them
The EHRs themselves are tools that can be used to make sure patients get what they need from their medical treatment. These records are much easier for medical personnel to use than paper records because they grant fast access to everything they need to know about a patient. When medical treatment is needed quickly, or when a specialist is consulted and results make a big difference in treatment, being able to send and receive records almost instantaneously can be highly valuable. The EHR companies know this, but they also know that they have to get things right. If their record software doesn’t work, patients’ lives can be at risk.
The Medical Staff and Their Use of Electronic Health Records
Medical staff who are switching over from paper records to EHRs can and do make mistakes. While medical information is rarely relatable in multiple choice verbiage, many of the EHR systems work off of dropdown menu options. Often times, healthcare professionals are forced to choose the closest answer, leaving room for misinformation and misinterpretations that can cause serious medical mistakes. Day-to-day typos and mistakes made in copying and pasting dates, dosages, and other patient information into EHRs are also possible. While these kinds of problems can happen to anyone no matter how long they have been using EHRs, people who are adapting to a new way of storing, using, and retrieving patient information are most likely to end up with errors. The culpability of the medical staff has to be considered carefully, because patients generally focus on the medical staff when issues appear. The idea that a patient would blame the EHR company for medical record errors is generally unlikely, and the medical staff would be the target of accusations, lawsuits, and related concerns.
The Health Insurance Portability and Accountability Act (HIPAA) affirms that the healthcare provider is the entity solely responsible for maintaining the integrity of the medical record, basically leaving the EHR vendor, consultant and systems integrator off the hook. Further, many EMR vendors include clauses in their contracts charging the physician with the responsibility to ascertain proper use and maintenance of the chosen EHR system.
Medical mistakes and malpractice issues can come about quickly, and those issues don’t have to be just related to a procedure. These kinds of concerns can also stem from HIPAA violations, incorrect recordkeeping, mishandled information, and similar topics. One inherent issue with electronic records in general is that they can experience connectivity problems, system crashes, and security breaches, leading to total shut down of a facilities health information system, as experienced by the Washington Medical Center MedStar Health, Inc. network in March 2016.
An additional patient complaint about EHRs is the perception that medical staff have an easier opportunity to falsify, manipulate, or even delete records that prove crucial in a medical malpractice case. Because of this, some courts question the validity of EHRs and can require that the records be tested before they are viable in court. Due to the relatively new technology that EHRs offer, courts have not yet had time to determine who may be at fault when patients bring a lawsuit based on EHR mistakes or misuse. Until more time has passed and more attorneys and courts have worked through patient concerns regarding EHR, culpability may not become completely clear.
An available option to help persons determine the integrity of their records in litigation is for the attorney to request an EHR audit trail. An EHR audit trail is a record detailing when a computer system was accessed, who accessed the system and what operations were performed. Simply put, the most common audit trail function is access management. Audit trails are also used for tracking the behavior of persons who access the EHR system, identifying computer failure sites and times to allow for data reconstruction, reviewing a systems ability to perform its functions (e.g., overload detection) and scanning for external intrusions of those unauthorized to enter organizational databases.
The Importance of Culpability
Culpability is extremely valuable and important in the medical and legal fields. The risk for lawsuits and other problems is high for doctors and their staff members. In a medical malpractice lawsuit, it’s crucial to sort through a patient’s electronic medical records in an efficient and reliable way in order to ensure your cases’ success. For patients who feel that they were treated unfairly or that their medical or personal information was compromised, understanding who may be responsible and liable is important.
Should Changes Be Made to the Current System?
Whether changes need to be made to the system is a discussion that’s still up for debate. EHR companies don’t want the culpability for potential misuse of their products. In turn, the medical professionals and staff want to be able to trust the tools they use. Clear-cut, direct culpability cannot really be determined for EHR, mostly because there are definitely two sides to the issue. That is why many insurers and attorneys are choosing to utilize the assistance of legal nurse consultants. Legal nurse consultants have the expertise needed to research and sort through these complicated records, find missing information and decipher errors in order to help define a case’s direction and probable outcome.
Identifying Medical Malpractice Expert Witnesses
Monday, June 6th, 2016
Sometimes medical negligence is apparent without need for explanation. It doesn’t take an expert to find fault when someone operates on the wrong limb or administers the wrong medication to a nursing home resident.
If medical professionals are the only ones with control over a negative outcome, and when an adverse event could only have been caused by a medical error, our legal system invokes the doctrine of res ipsa loquitur (Latin for “the thing speaks for itself.”) Simply stated, res ipsa is the principle noting that an event could have happened only due to negligence.
Although personal injury laws and rules of evidence are determined at the state level, the elements of res ipsa are pretty standard. For a case to meet the doctrine of res ipsa loquitur, three factors must be present: 1) the event would not occur in the absence of negligence; 2) the evidence of negligence rules out the possibility that the plaintiff’s actions caused the adverse event; and, 3) the negligent act occurs within the context of care provided by the defendant. It is often recommended that an expert witness be consulted, even in a case of res ipsa. The defendant’s attorney will usually challenge the notion that he or she had complete control over the circumstances.
In most cases of medical or nursing home negligence, expert witnesses are necessary to move a case forward. Lack of expert testimony can mean an early decision in an opponent’s favor – if not an outright dismissal. The facts and language of medicine are often too complex to understand. The appointed expert will walk the jury through the maze of medicine to understand why a lawsuit was filed in the first place.
Most states require plaintiffs to consult an expert witness to determine if the medical care provided to the plaintiff met the standard of care. In the legal arena, the standard of care is the level at which the average, prudent provider in a given community would practice. It is how similarly qualified practitioners would have managed the patient’s care under the same or similar circumstances. The standard of care is not necessarily the best care – just the average level expected of any care provider.
When a case does require qualified professional expertise, both plaintiffs and defendants must hire someone to serve in the role of expert witness. For cases to be tried in Federal Court, the Federal Rules of Civil Procedure (Fed.R. Civ.P.), requires the selected expert to prepare a detailed report in addition to a list of the expert’s prior testimony and compensation.
Although some states follow the Federal Rules of Civil Procedure, others have different rules for dealing with experts. In some states, an expert witness will be deposed before trial so the opposing side can be fully prepared to counter his or her opinions. In others, like New York, a legal team is not required to disclose the name of the designated expert, but they do have to provide opposing counsel with the expert’s bibliography.
What Makes A Medical Professional An Expert?
You may ask, “What makes a medical professional an expert?” One legal dictionary defines an expert as “a person who through education or experience has developed skill or knowledge in a particular subject so that he or she may form an opinion that will assist the fact finder.”
Each state has its own definition of who may be designated as a medical expert. Some states require that professional experience must be current, either for a specified number of years or that the expert was practicing in a clinical setting at the time of the incident. A degree from an AMA or AOA-accredited medical school are common requirements, as is board certification in the experts’ area of expertise. An unrestricted medical license with no recent history of suspension or revocation is paramount. Many states mandate that potential experts must devote a certain percentage of professional time to an active clinical practice, to avoid earning the reputation as a “professional witness.”
Nurse expert witnesses typically need a B.S.N. and recent clinical expertise in the same area as the defendant, with no record of legal issues or board disciplinary actions. Certification in the expert’s nursing specialty is an added plus.
Some states adhere to different versions of a specialty rule, which requires experts to practice in the same field of medicine as the defendant physician or nurse. A state’s locality rule obligates claimants to prove, by expert testimony, the recognized standard of acceptable professional practice in the community where the defendant medical provider practices or a similar community. For example, many states require that potential expert witnesses in medical malpractice cases must come from the state in which the alleged incident occurred or from a state contiguous to the venue in which the alleged incident occurred.
In most state malpractice lawsuits, attorneys on both sides will know the witnesses’ identities before getting to trial. They will research each expert’s career from their education to their publications. Every statement in an article written or testimony in cases with similar issues will be carefully scrutinized. The legal team will research the facts on which each claim is based – gleaning all it can to uncover the weak link in an expert’s opinion.
How Can An Expert Witness Be Utilized?
Expert witnesses can be used in a variety of ways. A medical professional may appear before the court as a “fact witness.” A “fact witness” is called to explain the medicine to the judge and jury. His or her role is to provide “just the facts” about a case, with no opinion regarding the medical care provided.
In medical malpractice and nursing home litigation, causation is the common Achilles’ heel. The rub lies in two questions every medical malpractice suit must answer. First, did the defendant fail to follow the standard of care for professionals in his or her position?
To answer this, a plaintiff-appointed expert may cite medical board guidelines or publications. What would industry standards expect of the defendant? How would a conscientious colleague with the same training treat this patient? What issues would that medical professional check for, and how would those issues be treated if diagnosed? An expert witness need not practice a higher standard of care than the defendant. He or she must only be conversant enough to determine that this standard was not followed.
The second question is thornier. If there was a breach in the standard of care, did this breach cause the negative outcome or damages? Given all the factors present, how likely was the plaintiff’s injury a result of substandard care?
The plaintiff’s goal is to find an expert who believes there is evidence of a breach of the standard of care. The defense will use its own expert to establish that the standard of care was observed – or that any deviation did not directly or proximately cause the adverse event. The plaintiff’s attorney, in turn, will get to work uncovering every possible way to challenge the defense’s expert testimony.
Finding properly credentialed healthcare professionals who are willing to offer opinions is not always easy. So what’s the best way to choose an expert witness? By consulting one.
Here is where a nurse’s expertise is of particular value. Upon studying the files and medical reports, this uniquely qualified consultant can recommend appropriate specialists.
Nursing expertise is ideal in complex cases of medical and care negligence. Identifying the probable cause of a medical event takes more than simply checking blood pressure and vital signs. A nurse is interested not only in physical agility but whether the patient has followed doctors’ and therapists’ directives and asked for assistance when necessary. This expert not only researches a patient’s diet, but whether or not the patient has adhered to the diet or eaten the food provided in a hospital or care facility. He or she would review physician progress notes, consultation reports, nursing progress notes, patient teaching records, lab results for specific issues and medication history for germane clues.
Legal nurse consultants (LNCs) are generally brought in to determine the merit of a case. Some help attorneys formulate questions to be asked at a deposition or trial. Some LNCs provide both consultation and testimony, while others prefer to work “behind the scenes.”
LNCs play a vital and advantageous role finding other experts for the case – from M.D. specialists to ancillary professionals like physical therapists, respiratory therapists, and pharmacists. Nurse expert witnesses are expected to testify at a deposition and trial if needed. Unlike the LNC consulting expert, the testifying expert may or may not be required to put their opinion in writing.
Both consulting LNCs and nurse expert witnesses review medical records and deposition testimony and formulate their conclusions. They commonly organize pertinent medical records and prepare record chronologies or timelines. They may also research medical and nursing literature and standards germane to issues in the suit brought forth. Both kinds of experts offer their own unique value to legal teams – and are often hired by healthcare organizations as risk managers or compliance experts.
As with other litigation, medical malpractice and long-term care cases often pit one expert against the other. Sometimes the tipping point in a jury’s decision is how well one witness can translate technical intricacies in to language they understand. ALN Consulting’s team of nurse consultants are in a unique position to build the strongest, most manageable court case for their clients – and boil medical-legal issues down to their essence. Contact us to learn how!
CMS Interpretive Guidelines – Revision to Feeding Tube Guidance
Wednesday, March 23rd, 2016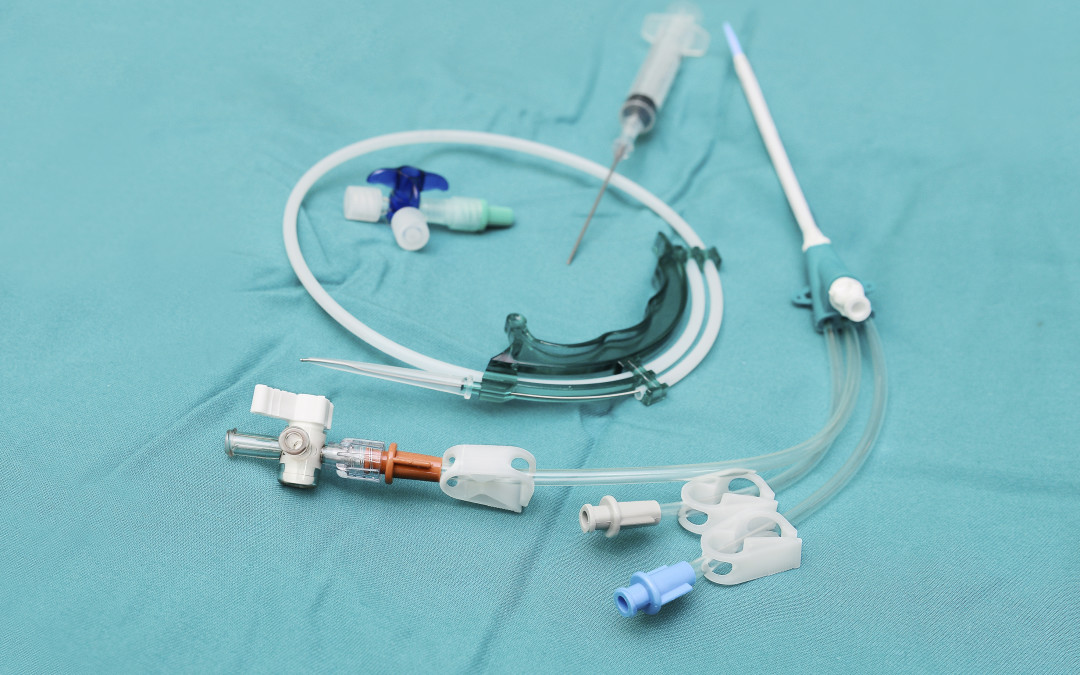
In this installment of the ALN Consulting series on the CMS Interpretive Guidelines, we explore the most recent revisions to surveyor guidance on feeding tubes in long-term care facilities. The Interpretive Guidelines include an explanation of the intent of the law, definitions of related terms, and instructions to surveyors on how to determine compliance with the law.
The CMS Interpretive Guidelines for Nasogastric tubes updates clarify expectations for long-term facility accountability in regards to use of feeding tubes; requiring that the resident’s legal representative be properly informed, specifying how nutritional needs are monitored, and mandating that potential risks associated with feeding tubes be considered in the decision making process.
The key to a strong defense against complaints related to long-term care residents’ nutritional status, particularly those who have feeding tubes, lies in a solid understanding of these guidelines and the recent revisions.
42 C.F.R. §483.25(g) Nasogastric Tubes (F tag 322)
The CFR Regulation states, “Based on the comprehensive assessment of a resident, the facility must ensure that:
- A resident who has been able to eat enough alone or with assistance is not fed by nasogastric tube unless the resident’s clinical condition demonstrates that use of a nasogastric tube was unavoidable; and
- A resident who is fed by a nasogastric or gastrostomy tube receives the appropriate treatment and services to prevent aspiration pneumonia, diarrhea, vomiting, dehydration, metabolic abnormalities, and nasal-pharyngeal ulcers and to restore, if possible, normal eating skills.”
Relevant definitions in the Interpretive Guidelines include:
Avoidable: There is not a clear indication for using a feeding tube, or there is insufficient evidence it provides a benefit that outweighs associated risks.
Unavoidable: There is a clear indication for using a feeding tube, or there is sufficient evidence it provides a benefit that outweighs associated risks.
Bolus feeding: The administration of a limited volume of enteral formula over brief periods of time.
Continuous feeding: The uninterrupted administration of enteral formula over extended periods of time.
Enteral nutrition (a.k.a. “tube feeding”): The delivery of nutrients through a feeding tube directly into the stomach, duodenum, or jejunum.
Feeding tube: A medical device used to provide enteral nutrition to a resident by bypassing oral intake.
Gastrostomy tube (“G-tube”): A tube that is placed directly into the stomach through an abdominal wall incision for administration of food, fluids, and medications. The most common type is a percutaneous endoscopic gastrostomy (PEG) tube.
Jejunostomy tube (a.k.a. “percutaneous endoscopic jejunostomy” (PEJ) or “J-tube”): A feeding tube placed directly into the small intestine.
Nasogastric feeding tube (“NG tube”): A tube that is passed through the nose and down through the nasopharynx and esophagus into the stomach.
Transgastric jejunal feeding tube (“G-J tube”): A feeding tube that is placed through the stomach into the jejunum and that has dual ports to access both the stomach and the small intestine.
Tube feeding (a.k.a. “enteral feeding”): The delivery of nutrients through a feeding tube directly into the stomach, duodenum, or jejunum.
Regulation Tag F 322
The feeding tube requirement has two parts. The first aspect requires that the facility utilize a feeding tube only after it determines that a resident’s clinical condition demonstrates this intervention was unavoidable. The second aspect requires that the facility provides to the resident who is fed by a tube services to prevent complications, to the extent possible, and services to restore normal eating skills, if possible.
The facility is in compliance with 42 CFR §483.25(g), if staff:
- Uses a feeding tube to provide nutrition and hydration only when the resident’s clinical condition makes this intervention necessary based on adequate assessment, and after other efforts to maintain or improve the resident’s nutritional status have failed;
- Manages all aspects of a feeding tube and enteral feeding consistent with current clinical standards of practice in order to meet the resident’s nutritional and hydration needs and prevent complications; and
- Identifies and addresses the potential risks and/or complications associated with feeding tubes, and provide treatment and services to restore, if possible, adequate oral intake.
Surveyor “Probes” in Facility Use of Feeding Tubes
Probes, or questions posed by the Interpretive Guidelines for surveyors, can be used by the defense team to bolster evidence that a practitioner or facility met the standard of care. There are many probes in F tag 322 related to resident rights; technical and nutritional aspects of feeding tubes; care of the feeding tube; and complications related to the feeding tube and/or the enteral nutrition product. Some examples of surveyor probes include:
- Was the resident and/or the resident’s legal representative informed about the relevant benefits and risks of tube feeding?
- How has the staff and practitioner determined the cause of decreased oral intake/weight loss or impaired nutrition and attempted to maintain oral intake prior to the insertion of a feeding tube?
- How did the staff determine the resident’s nutritional status was being met, such as periodically weighing the resident, and how did they decide whether the tube feeding was adequate to maintain acceptable nutrition parameters?
- How has the facility identified the resident at risk for impaired nutrition, identified and addressed causes of impaired nutrition, and determined that use of a feeding tube was unavoidable?
- How has the staff verified that the feeding tube was properly placed?
- How has the staff monitored a resident for possible complications (e.g., diarrhea, nutritional deficits, aspiration, depression, withdrawal, etc.) related to a feeding tube and the tube feeding, and how have they identified and addressed such complications?
Updates to the Interpretive Guidelines
The Interpretive Guidelines entitled Nasogastric tubes was vastly updated in November 2014. For the purpose of the guidelines, the regulatory title is considered to include any feeding tube used to provide enteral nutrition to a resident by bypassing oral intake. (Since the regulation was created use of actual nasogastric tubes have become rare, and use of other types of enteral feeding tubes have become more prominent.)
The newest guidance stresses the unavoidability standard, and also emphasizes quality of life and resident choice. Based on the guidelines, it could be argued that some examples of possible adverse effects from feeding tubes such as diminished socialization and loss of the experience of taste, texture, and chewing must be considered as important, and may possibly outweigh the benefits of feeding tubes such as preventing malnutrition and dehydration, and aiding wound healing. A new statement regarding the use of feeding tubes in elderly patients with dementia also addressed the controversy in this arena. “The literature regarding enteral feeding of these individuals suggests that there is little evidence that enteral feeding improves clinical outcomes (e.g., prevents aspiration or reduces mortality).”3
In the defense of the use, non-use, or complications of feeding tubes, the Interpretive Guidelines; Nasogastric tubes now provide a much larger framework for the difficult end of life decisions which are inherent in turning towards non-oral sustenance. With the comprehensive updates added to this guideline, ALN Consulting can help your defense team pinpoint crucial, relevant prompts and research to strengthen a case with complaints involving tube feeding.
References
- Harris, Rick E. (2015). How to Use the CMS Surveyor Guidance to Craft a Winning Defense [Presentation at the DRI LTC/SNF Seminar].
- Centers for Medicare & Medicaid Services. (2015). State Operations Manual – Appendix PP – Guidance to Surveyors for Long-term Care Facilities. Retrieved 02/23/16.
- Compliance Solutions for the Perfect Survey Every Day. (2014). F322. Retrieved 02/23/16 from The Perfect Survey website.
